Originally published 8/6/2015
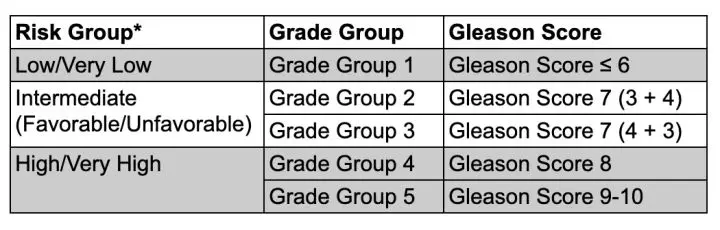
In 2014, the International Society of Urological Pathology released a proposed new prostate cancer (PCa) grading system, called the Grade Groups (GG). Our initial blog on the topic (below) explains some of the reasoning behind simplifying the traditional Gleason scoring system—a sum of two numbers—into a more understandable 5-point aggression scale as this table shows:
This new system is now widely used. It is more elegant in its simplicity, but doesn’t account for specific clinical factors that are linked with greater risk of early treatment failure (biochemical recurrence, or BCR). In a 2021 correlation of GG with these factors, Okubu et al. take the GG system a step further: “In addition to GG, other important indices of malignancy were determined and weighted…”[i]
Their study was based on 299 radical prostatectomy (RP) cases for which full case records and surgical pathology reports were available. To determine what, in addition to GG 5, predicts early BCR, they included pre- and post-RP parameters: patient age; PSA at diagnosis; tumor diameter; invasiveness (lymphatic, seminal vesicle, neurovascular bundle); extraprostatic tumor extension; positive surgical margins; and lymph node metastasis. They used statistical methods to correlate each factor with each GG level. Here is a sample of their findings:
- Lymphatic invasion rate increased from GG 3 and reached a plateau at GG 4 • Extraprostatic extension was detected at a constant frequency starting at GG 2 but became extremely high at GG 5
- Seminal vesicle invasion had a sharp increase at GG 5
- Venous invasion rates began to rise at GG 4 and were even higher at GG 5.
Tumor diameter was significantly linked with GG 5. The authors state that “we would like to raise a possibility that GG and tumor diameter may have implications as risk factors for very early BCR.” They note that their findings did not find lymph node metastasis to be a significant predictor of early BCR, but other studies have indeed found this to be so. The work of Okubu, et al. enriches and refines the GG system in terms of its value as a prognostic tool. We encourage interested readers to take advantage of the full paper for their results.
In the 1960s, a pathologist named Donald Gleason and his colleagues at the Minneapolis VA Hospital developed a numerical system for ranking prostate cancer (PCa) aggressiveness on a scale from 1 to 5. The Gleason grade (or Gleason score) system named after him have been in use ever since as a way to understand how aggressive a patient’s PCa disease is, and planning treatment accordingly.
Now, 17 experts from Johns Hopkins, Memorial Sloan Kettering, U Pittsburgh, Cleveland Clinic, and Sweden’s Karolinska Institute propose a simplified 5-point system.[ii] Their thinking is based on analyzing the records of more than 26,000 patients (20,845 had prostatectomy, 5501 had radiation).
When is a 7 not a 7?
The alternate system would have the advantage of simplicity. Today’s Gleason grade is not a true 5-point scale because it involves summing up two values. Which number comes first is based on the largest per cent of PCa seen in each positive needle sample. Thus, Gleason 3 + 4 = 7 is different from Gleason 4 + 3 = 7; the second sum is more dangerous because there is more Gleason 4 than 3. Even though the Gleason system is based on numbers 1 through 5, the actual scale used is this:
3 + 3 = 6 (lowest grade PCa)
3 + 4 = 7
4 + 3 = 7
4 + 4 = 8
4 + 5 = 9
5 + 4 = 9
5 + 5 = 10
It’s really a 7-point scale. The authors state, “The lowest score, assigned 6, may be misunderstood as a cancer in the middle of the grading scale, and 3+4=7 and 4+3=7 are often considered the same prognostic group.” (Note that any sum less than 6 is not used for planning treatment.) Confusing, right?
Why would a new system be better?
A true 5-point scale can offer the smallest number of grades with “more accurate grade stratification.” This simplifies treatment planning. According to the authors, if the lowest grade is 1 instead of 6 (3 + 3), the current tendency to overtreat low-risk PCa can be greatly reduced.
I like the 5-point scale, an idea similar to the PI-RADS scoring system radiologists use to interpret multiparametric MRI prostate scans. (See my blog at https://sperlingprostatecenter.com/pi-rads-score/ to learn more.) Given the tendency of the medical profession to change slowly and cautiously, I don’t foresee rapid wide-spread adoption of a new system. However, the authoritative institutions and experts behind this study should help their proposal gain the consideration it well deserves. I expect that there will be quite a buzz about it at next year’s annual American Urological Association meeting.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Okubo Y, Sato S, Osaka K, Yamamoto Y et al. Clinicopathological Analysis of the ISUP Grade Group And Other Parameters in
Prostate Cancer: Elucidation of Mutual Impact of the Various Parameters. Front Oncol. 2021 Jul 28;11:695251.
[ii] Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB et al. A Contemporary Prostate Cancer Grading System: A Validated Alternative to the Gleason Score. Eur Urol. 2015 Jul 9. pii: S0302-2838(15)00557-6. doi: 10.1016/j.eururo.2015.06.046.