I’ve been noticing some confusion among patients over the traditional Gleason score system and the new Gleason Grade Group system. I figured it’s time for a quick review and refresher course. You’ll be relieved to know there are no quizzes, midterms or final exams! However, it’s all about grades—but not the kind you get in school.
When it comes to prostate cancer (PCa), perhaps the single most important thing a patient should know is the degree to which his PCa is dangerous. This degree is expressed as a numeric value, or grade. The higher the number, the greater chance that his disease has lethal potential. Just as with most academic grading systems, there is a 5-level scale. In school, even young kids learn catch on right away:
| Academic Grades | Prostate Cancer Grades |
|
A = Well above average B = Above average C = Average D = Below average (in danger of flunking) F = Definitely flunking |
1 = Normal 2 = Not so normal (suspicious of cancer) 3 = Cancer (does not look dangerous) 4 = Cancer (suspicious of danger) 5 = Cancer (definitely dangerous) |
Traditional Gleason score
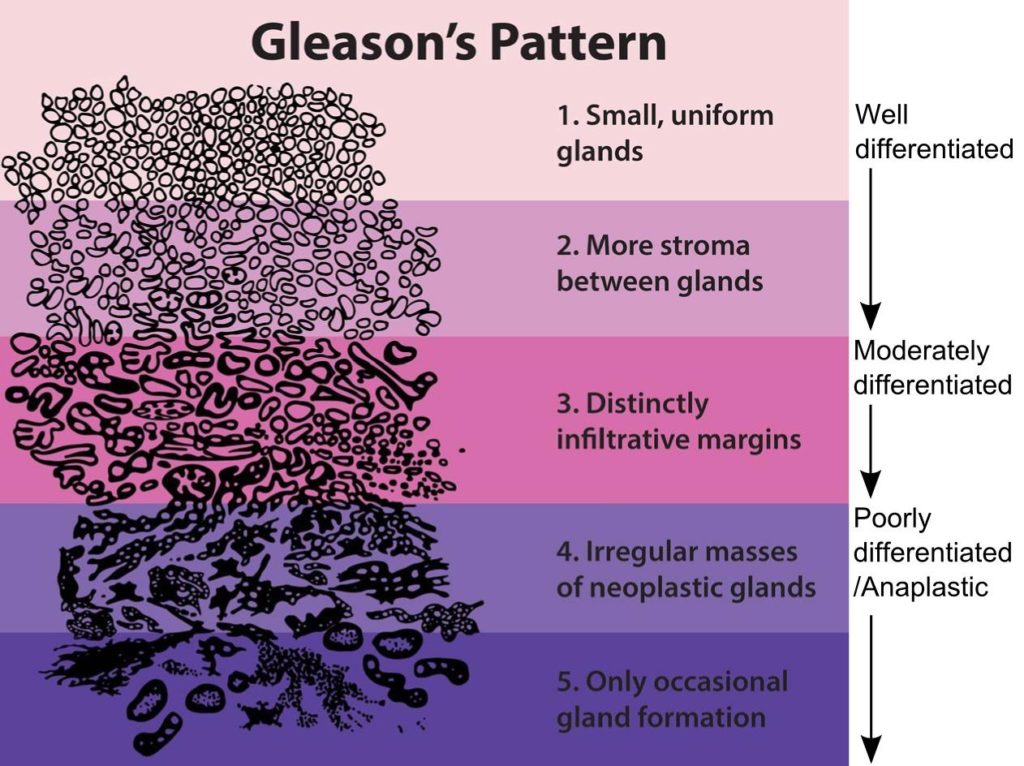
When you think of prostate cancer tumors, the word “architecture” likely does not come to mind. However, Dr. Donald Gleason, a pathologist at the Minneapolis VA Medical Center, approached the challenge of developing a standardized description of prostate cancer (PCa) aggression according to the appearance of PCa cellular architecture under a microscope. He created a 5-point scale in which the higher the score, the more the structure has the undifferentiated appearance of potentially lethal PCa, as this graphic shows[i]
As you see, a score of 1 indicates normal prostate cell structures (well differentiated, indicating no cancer). Then, as the colored areas deepen in intensity, you can see it becomes increasingly chaotic. Using this as a guide, pathologists examining biopsy tissue samples can assign scores.
Gleason scores are presented as a sum of two numbers, e.g. Gleason score 3+3 = 6, or Gleason score 4+3 = 7. The reason for this was to give a richer description of a patient’s PCa according to the two largest cancer amounts picked up by the biopsy needles. The first number is the larger amount, and the second number is the next larger amount. Thus, 3+3 = 6 is another way of saying the tumor is “moderate plus moderate = moderate”, while 4+3 is another way of saying “more dangerous + moderate = more dangerous”, because the larger volume of identified PCa is more dangerous.
The system, of course, is not foolproof. Two different pathologists looking at the same tissue samples might not agree, especially when it comes to distinguishing a 3 from a 4. Thus, patients are commonly advised to get at least one more pathology opinion on their slides. However, the system is more than adequate for giving doctors a way to explain to a patient why he’s recommending one or more treatments that are matched to the score, plus it’s useful for research/statistical studies.
The new Gleason Grade Group (GG) system
The two-number system was often perplexing to patients. Therefore, in 2014 the International Society of Urological Pathologists (ISUP) proposed a revision, grouping PCa architecture by risk level. The table below shoes the Risk Group, the Grade Group, and how it parallels the 2-number Gleason score:
| Risk Group | Grade Group | 2-number Gleason Equivalent |
| Low | Grade Group 1 | Gleason score ≤ 6 |
| Intermediate favorable | Grade Group 2 | Gleason score 3 + 4 = 7 |
| Intermediate unfavorable | Grade Group 3 | Gleason score 4 + 3 = 7 |
| High | Grade Group 4 | Gleason score 8 |
| High | Grade Group 5 | Gleason score 9-10 |
The Prostate Cancer Foundation notes, “Many hospitals report both the Gleason score and the Grade Group, but there may be hospitals that still report only the old Gleason system.”[ii]
I hope this brief exploration of how PCa is scored or graded helps to clarify the meaning of the numbers. We are still in a transition from the original 2-number score, but as more researchers and clinicians are turning to the simpler risk-level basis, it will become simpler for patients to identify what they’re dealing with.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Public Domain, https://commons.wikimedia.org/w/index.php?curid=440437
[ii] https://www.pcf.org/about-prostate-cancer/diagnosis-staging-prostate-cancer/gleason-score-isup-grade/