Location, location, location! No, this is not a blog for homebuyers. Rather, it’s about testosterone in a man’s blood supply.
Testosterone is the major male hormone (androgen) in a man’s body. It’s his biochemical best friend. It is essential to male characteristics like sex drive, muscle mass, sperm production, etc. A man’s testosterone or T level is determined by a simple blood test. That’s because T produced in the testicles circulates throughout the body’s arteries, veins, and tiny blood vessels called capillaries. This wide blood supply is called peripheral blood, and blood drawn from any vein gives a consistent peripheral T level. A simple review reminds us that arteries carry oxygenated blood away from the heart to distribute oxygen and other nutrients everywhere, while veins return the used-up blood and waste products to the heart.
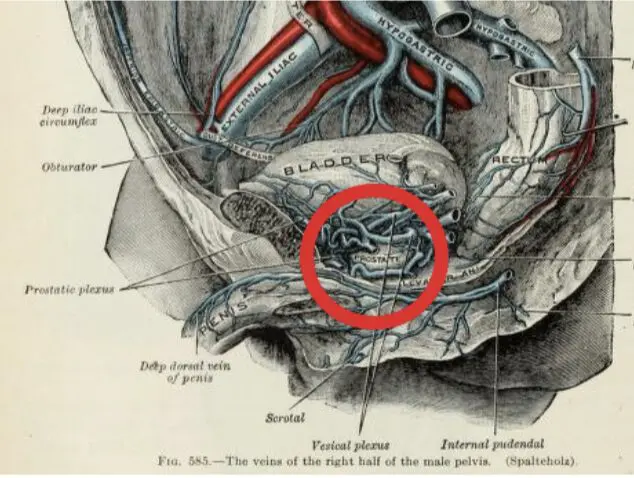
However, each man’s body is slightly unique. This is true of how his prostate anatomy operates, including the local vein systems that receive the used blood from prostate and other structures. They are small, deeply embedded streams that eventually meet up like a river to channel it back to the heart. A specific system is the prostatic dorsal venous complex (DVC). The illustration below[i] shows the complicated veins surrounding the prostate, which is barely visible in the center of the red circle:
Peripheral blood vs. prostatic blood
Now, to return to the topic of testosterone location, I’ve already established it’s widely circulated at a consistent level throughout the body. However, a new study offers a startling revelation. Some men have a higher T concentration in the prostatic blood than in the peripheral blood. A regular blood test (peripheral blood) for T level will NOT detect this! However, it’s not possible before prostate cancer (PCa) treatment to get a needle blood draw from the prostatic DVC to compare local with peripheral T levels. This is unfortunate because there are grave implications for prostate cancer (PCa) patients who have this concentration.
Important breaking news
Traditionally, it’s been thought that T levels in peripheral blood mirror T levels in prostatic blood. It turns out that this is NOT the case for about a fifth of PCa patients! A Sep. 1, 2023 study published by the Journal of Clinical Observation tells us that PCa patients whose DVC blood has an enriched testosterone appear to have more aggressive PCa, which is more likely to come back even after surgical removal[ii].
The evidence comes from 266 PCa patients who had radical prostatectomy (RP) to remove their glands. During the surgery, the clinical team had access to the DVC to collect local blood samples. Peripheral blood samples were also collected, and after the surgeries, “Tissue samples from 170 prostates were analyzed, and data were available for assessment of clinical outcomes for 209 men.”
Once the blood samples were analyzed for T levels and other steroids, what the authors found was astonishing, contradicting the belief that peripheral male hormones always reflect prostate exposure: A substantial proportion of the men with prostate cancer had periprostatic T levels that far exceeded the corresponding levels in the peripheral circulation. Approximately 20% of men had local T concentrations at least 2-fold higher than peripheral T, and approximately 5% of men had at least a 10-fold elevation of periprostatic T levels.
Even more remarkable, these findings are independent of independent of pre-treatment clinical factors, including PSA and biopsy findings! Thus, the authors have dubbed this “sneaky testosterone” because with today’s clinical methods, it’s not possible to know in advance which PCa patients are victims of this condition. A peripheral blood draw does not pick this up. As such, it’s not possible to plan the right treatment match. The only way to diagnose this situation is after RP, during which prostatic blood must be routinely sampled. As the authors write,
The potential implications for this finding are broad and profound. In men who already have androgen-dependent prostatic diseases such as benign prostatic hyperplasia or prostate cancer, knowledge of the absence, presence, and extent of this ‘sneaky’ T physiology and total prostatic androgen exposure may further clarify an individual’s distinct natural history of the disease.
This is truly new information that bears on treatment planning for localized PCa. As the authors conclude, “… findings of an alternative local endocrine physiology have broad potential implications for the assessment of risk in diseases of the prostate and implicate potential alternative treatment strategies for urologic diseases that are modulated by sneaky T physiology.” We will report further research on how to integrate these findings in diagnosing PCa risk levels. Stay tuned.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you have health concerns or questions of a personal medical nature.
References
[i] Gray’s Anatomy (20th edition), p. 674. 1918 (in the public domain).
[ii] Alyamani M, Michael P, Hettel D, Thomas L et al. Elevated periprostatic venous testosterone correlates with prostate cancer progression after radical prostatectomy. J Clin Invest. 2023 Sep 1;133(17):e171117.


