According to statistics, not all men with prostate cancer are created equal. Statistics from the National Institutes of Health tell a sad tale: black men have about a 1.5 – 2 times greater chance of developing prostate cancer (at least 15% vs. 10% respectively; are more often diagnosed with aggressive PCa; and the risk of PCa-specific death is nearly twice as great. Why is this?
The largest PCa case record study to date concluded that lack of access to equal healthcare explains more than biology alone.[i] Yet other studies do show evidence of biological disparities in the genes. A 2017 research team wrote that the problem of prostate health disparity is complex: “The risk factors that drive this disparity are unknown and potentially consist of social, environmental, and genetic influences.”[ii] The study they conducted specifically explored the genetics of PCa in black men.
In their genomic analysis they identified two chromosomes with risk-associated mutations “only in men of African ancestry.” They use a neutral phrase (I emphasize it in bold): “These findings provide further support for the role of ancestry-specific germline variation in contributing to population differences in prostate cancer risk.” I prefer their precise choice of words over the idea of racial differences, since science tells us we are all one race. Another example of ancestry-specific germline variation is Tay-Sachs disease, with a disproportionate incidence among Jewish people of Ashkenazi descent.
Ancestry-specific PCa vulnerability
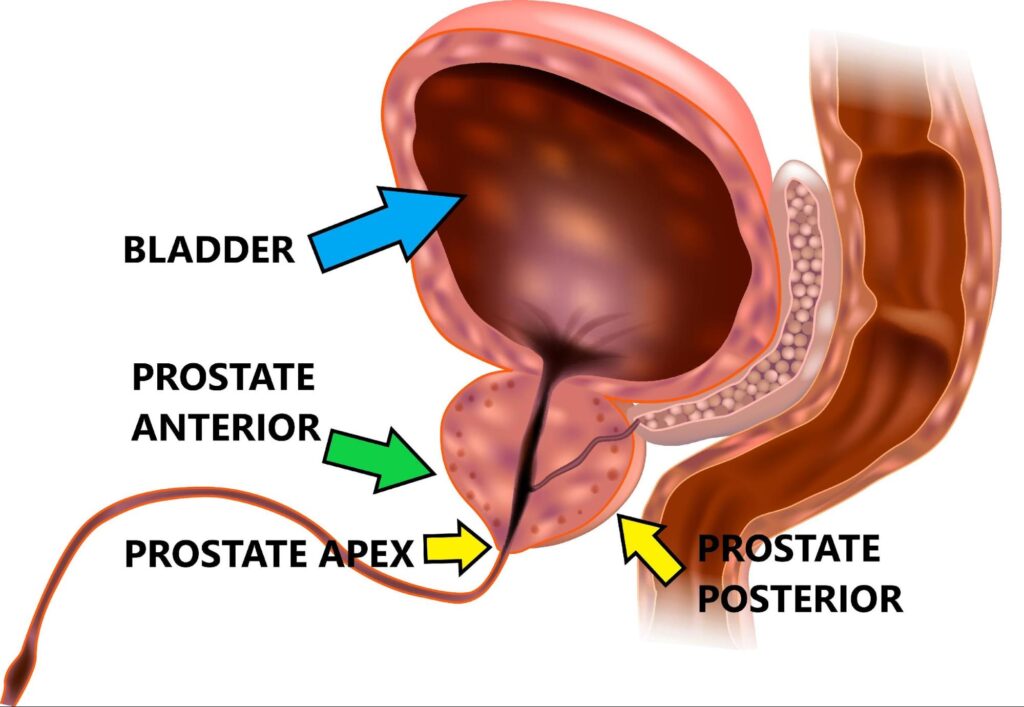
Evolution and ancestry account for an untold number of gene variants that manifest in population vulnerabilities for certain diseases. This, plus unequal healthcare, appears implicated in statistical PCa disparity. I was intrigued by a 2014 study[iii] demonstrating that black men have higher probability than white men of tumors in the anterior (toward the front) region of the gland:
Anterior zone (AZ) tumors are especially concerning because conventional 12-core TRUS-guided biopsies tend to miss tumors in that location, and AZ tumors tend to have poor pathologic features across all patient groups. This study, involving prostatectomy patients initially diagnosed with low-risk PCa by minimum 10-core TRUS biopsies, used post-surgery gland specimens from 89 white men and 87 black men to analyze tumor volume, grade and location. The researchers found that regardless of initial biopsy results, after surgery black men were more likely to be found to have:
- significant prostate cancer (61% vs 29%)
- Gleason 7 or greater (37% vs 11%,)
- volume of greater than 0.5 cm (45% vs 21%)
- larger dominant nodules (median 0.28 vs 0.13 cm)
- anterior location of any PCa (51% vs 29%)
- anterior location of dominant nodule that had a higher Gleason score than indicated by biopsy (59% vs 0%, p = 0.001)
To remedy this, the authors suggest that “enhanced imaging or anterior zone sampling may detect these significant anterior tumors, improving the outcome in black men [especially in those] considering active surveillance.” I agree, and would add, improved outcomes for black men considering any treatment.
Multiparametric MRI
Experts agree that during active surveillance (AS), monitoring biopsies should be particularly directed to the anterior zone (AZ) since men diagnosed with low-risk (grade group 1) PCa—not just black men—harbor higher-grade cancers in at least 25% of cases, often located in the AZ. However, many of these biopsies could be avoided, and anterior disease detected earlier, by noninvasive multiparametric MRI (mpMRI) before biopsy. PCa expert Laurence Klotz writes,
Failure to identify these cancers early in the pre-MRI era likely was responsible for most of the metastatic progression events in grade group 1 surveillance patients, and early identification of these ‘wolves in sheep’s clothing’ is likely to further reduce the metastasis rate …[iv]
A 2019 paper by Walton, et al.[v] is devoted to PCa detection in black men using mpMRI targeted biopsy. Both white and black men were included in the study group, all of whom had initial mpMRI scans read by a single radiology group using PI-RADSv2 (scale of 1 to 5) to categorize lesions. 125 patients were included, and 214 lesions were detected among them (64 in black men, 150 in white men). Following detection and scoring, mpMRI-targeted biopsies were performed to determine cancer detection rates.
Notably, this study found no significant differences between white and black patients in terms of tumor locations which were distributed proportionately. According to the authors:
The overall cancer detection rate was 50%, which did not differ significantly between prostate zones or racial groups. The cancer upgrade rate was 41% and it also did not differ significantly between prostate zones or racial groups.
However, the 48 anterior lesions detected had a higher average cancer detection rate, higher PI-RADS score, tended toward larger size and upgrading. The authors concluded that “magnetic resonance imaging targeted biopsy is equally effective in African American and Caucasian men…”
We don’t yet know if a “great equalizer” for PCa conditions will emerge. For now, it appears that mpMRI is a helpful step forward in correcting ancestral PCa vulnerabilities between population groups.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Dess RT, Hartman HE, Mahal BA, Soni PD et al. Association of Black Race With Prostate Cancer-Specific and Other-Cause Mortality. JAMA Oncol. 2019 Jul 1;5(7):975-983.
[ii] Conti D, Wang K, Sheng X, Bensen JT. Two Novel Susceptibility Loci for Prostate Cancer in Men of African Ancestry. J Natl Cancer Inst. 2017 Aug 1;109(8):djx084.
[iii] Sundi D, Kryvenko ON, Carter HB, Ross AE at al. Pathological Examination of Radical Prostatectomy Specimens in Men with Very Low Risk Disease at Biopsy Reveals Distinct Zonal Distribution of Cancer in Black American Men. J Urol. 2014 Jan; 191(1): 60–67.
[iv] https://www.practiceupdate.com/content/anterior-zone-biopsy-in-men-on-active-surveillance-for-prostate-cancer/63566
[v] Walton E, Yaguchi G, Keeley J, Deebajah M et al. Effect of Lesion Location on Prostate Cancer Detection Rate with Magnetic Resonance Imaging Targeted Biopsy in African Americans. J Urol. 2019 Mar;201(3):503-509