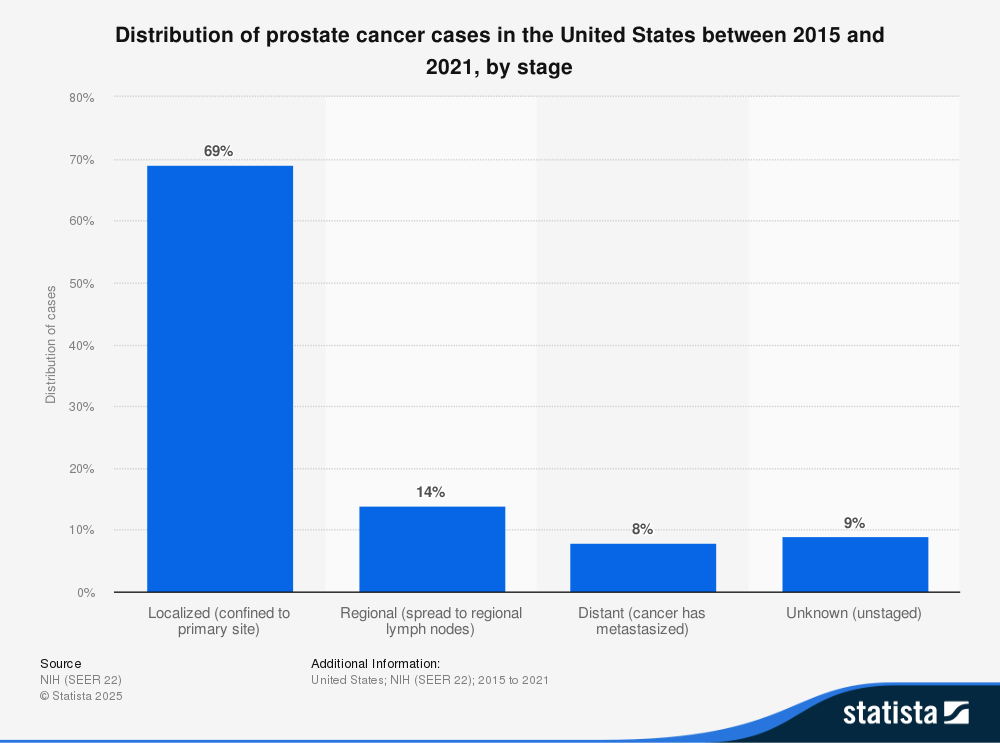
Prostate cancer (PCa) is the most common non-skin cancer in men. The American Cancer Society reports that over 300,000 new cases will be diagnosed in 2025. Of those, 69% are still localized.
Localized PCa means the cancer is still contained in the prostate gland. Since there is no one size-fits-all treatment, doctors and patients share the goal of conquering localized PCa with the least side effect impact. Precise diagnosis is a must to determine the best treatment match.
Customizing treatment for localized disease
Each PCa patient has a unique combination of clinical factors. Most important, of course, is an accurate physical portrait of the cancer. Tumor aggression level, size, extent, and genetic variants combine to help determine treatment method. Other physical factors include patient age, life expectancy, family history of cancer (especially prostate, breast and ovarian cancers), exposure to carcinogens, and other health problems. All physical characteristics are evaluated.
Detection and diagnosis are not the same
Detection means taking steps to find out if PCa is present:
- Step 1: For most patients, a high or rising PSA is the first clue. However, PSA is not specific for cancer. Other conditions such as BPH, prostatitis, even riding a bike or having sex before a blood draw can raise PSA. So, more clues are needed.
- Step 2: Before biopsy, have a multiparametric MRI (mpMRI) of the prostate done on a 3T magnet (high field strength) by an expert. Depending on tumor location, this test can visually rule PCa in or out. Studies like the one by Martins, et al. (2020) show that mpMRI is accurate, with positive prediction of 94% that PCa is present, and negative prediction of 97% that it is not.[i]
- Step 3 Substances called biomarkers that can be found in blood, urine or tissue also offer more specific PCa evidence. An important blood biomarker is PSA-density (PSA-d) that is used in combination with mpMRI for greater specificity.
Diagnosis means proof that PCa has developed in the prostate gland. For that, a needle biopsy is needed. Tissue samples are extracted by hollow needles for examination under a microscope. This is the only way to prove that cancer cells are present.
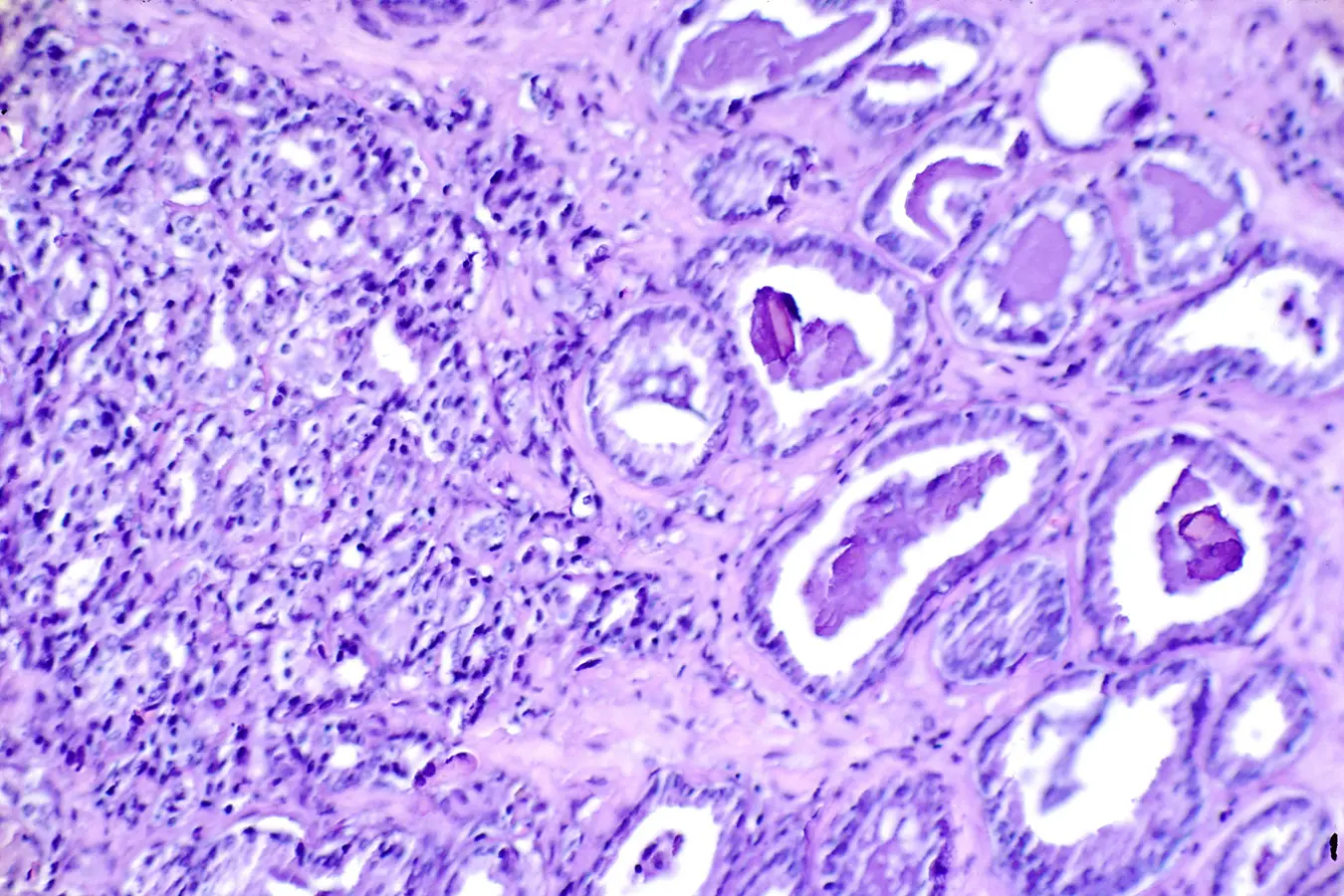 Biopsy slide reveals PCa. On the right is a Gleason Value of 3 (out of 5) with moderately differentiated cancer. On the left is less normal tissue with a Gleason Value of 4 (out of 5) that is highly undifferentiated. The Gleason score is the sum of the two worst areas of the histological slide. Photo courtesy of the website of the National Cancer Institute.
Biopsy slide reveals PCa. On the right is a Gleason Value of 3 (out of 5) with moderately differentiated cancer. On the left is less normal tissue with a Gleason Value of 4 (out of 5) that is highly undifferentiated. The Gleason score is the sum of the two worst areas of the histological slide. Photo courtesy of the website of the National Cancer Institute.
Most precise biopsy method
Before prostate MRI was developed, standard biopsies were guided by Transrectal Ultrasound (TRUS). Since TRUS does not reveal or define cancer tissue, doctors used 12+ needles to randomly sample the prostate according to a grid-like pattern. This approach has an error rate of 15-46%. Also, the risk of infection and biopsy side effects increases with the number of needles. Thankfully, experts have now shown that mpMRI before biopsy and MRI-guided targeted biopsy offer superior precision diagnosis over standard TRUS-guided biopsy.
This is because biopsy needles guided by real-time (in-bore) MRI are selectively targeted into suspicious lesions. The inner core is where the more dangerous cells are likely to exist, so the aggression level of the tumor is more accurately diagnosed. This overcomes the shortcomings of randomized TRUS-guided systematic biopsies.[ii] Typically, a real-time (in-bore) mpMRI guided biopsy requires 2-4 needles, reducing risks associated with TRUS-guided 12-14+ needle biopsy.
Together with mpMRI results, the cells seen from a biopsy give key information about the tumor: location and extent, how aggressive the cancer cells are (Gleason Grade Group) and the percentage of cancer cells in each needle positive for PCa. The treatment best suited to conquering localized cancer with the least impact on quality of life depends on accurate diagnosis, taking into account all other factors as described above. For the most precise biopsy, a few needles guided by real time in-bore MRI is simply the best.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Martins M, Regusci S, Rohner S, Szalay-Quinodoz I et al. The diagnostic accuracy of multiparametric MRI for detection and localization of prostate cancer depends on the affected region. BJUI Compass. 2020 Nov 28;2(3):178- 187.
[ii] O’Connor LP, Lebastchi AH, Horuz R et al. Role of multiparametric prostate MRI in the management of prostate cancer. World J Urol. 2021 Mar;39(3):651-659. doi: 10.1007/s00345-020-03310-z.