SUMMARY
Multiparametric MRI (mpMRI) with 3T technology provides unmatched accuracy in detecting clinically significant prostate cancer. At Sperling Prostate Center, Dr. Dan Sperling integrates MRI imaging with AI tools to determine which patients truly need biopsy and which can safely avoid it, ensuring precise diagnosis and personalized treatment planning.
A prostate cancer diagnosis can come as a shock. However, an accurate diagnosis is the key to successful treatment. For excellence in prostate cancer detection, diagnosis and treatment planning, the Sperling Prostate Center is second to none. Dr. Dan Sperling and his experienced team offer top tier MRI-based clinical prostate cancer services, starting with accurate detection.
Doesn’t a PSA test detect prostate cancer?
Not necessarily. The PSA (Prostate Specific Antigen) blood test is a screening tool to detect suspicion of prostate cancer, but it does not always mean cancer. It only detects a spike in prostate activity. While prostate cancer is abnormal activity, PSA levels can also be elevated due to several non-cancerous conditions like benign prostatic hyperplasia (BPH), prostatitis, recent sexual activity, etc.
As Dr. Sperling points out there are now sophisticated blood or urine tests that can reveal cancer biomarkers. These tests are more specific than PSA and can rule out benign conditions, but it is too soon to rush to biopsy. More advanced detection is the next step to clarify if a biopsy is truly needed.
Does Dr. Sperling offer more advanced detection specifically for prostate cancer?
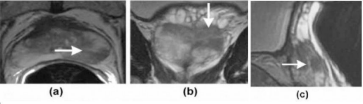
Yes. For advanced detection, Dr. Sperling uses multiparametric MRI (mpMRI) to detect clinically significant cancer (defined as Grade Group > 2). When done on his Center’s powerful 3T (3 Tesla) magnet, mpMRI can reveal if clinically significant prostate cancer (csPCa) is present and requires biopsy. The image below illustrates how mpMRI detects clinically significant prostate cancer (arrows).
Not every doctor is equally qualified to interpret a patient’s mpMRI scan. Studies show that experience matters. As stated in a 2024 published study, “Prostate MRI benefits from reader experience.”[i] Not only is Dr. Sperling a long-standing pioneer in prostate mpMRI, his ability to interpret a patient’s risk level is aided by Artificial Intelligence to improve risk stratification.[ii]
Can 3T mpMRI rule out clinically significant prostate cancer?
As done by Dr. Sperling, 3T mpMRI can rule out csPCa. If no csPCa is visible, it’s called a negative MRI. One analysis found an average negative rate of 93% for mpMRI on a 3T magnet.[iii] Another study found that mpMRI correctly ruled out csPCa with 94.2% accuracy.[iv]
The Sperling Prostate Center provides high-quality MRI technology with integrated AI tools. Dr. Sperling acquires top-quality images, correctly interprets them using the standardized PI-RADS reporting system, and integrates imaging results with other key clinical factors.
Even if mpMRI is negative, isn’t a biopsy still needed?
Dr. Sperling cites the latest research showing that when mpMRI is negative, a biopsy can safely be avoided. A high-level study found that “men with negative MRI results may not be at an elevated risk for prostate cancer and can safely avoid biopsy when appropriate monitoring measures are implemented.”[v]
Ongoing monitoring is important. Dr. Sperling recommends PSA tests at prescribed intervals, with mpMRI performed immediately if PSA is suspicious. This enables the earliest possible detection of potential csPCa.
If a biopsy is necessary, does Dr. Sperling’s biopsy approach differ from standard biopsies?
Yes, Dr. Sperling is a pioneer in real time MRI-guided targeted biopsy. It differs significantly from standard TRUS-guided biopsies. Note that a definitive diagnosis can only be made by a specialist who examines biopsy tissue under a microscope. This is why a biopsy is necessary if mpMRI detects csPCa.
Standard biopsies guided by real-time TRUS (transrectal ultrasound) take 12 or more needle samples. Since TRUS cannot distinguish between normal prostate tissue and suspected tumors, it is basically blind and random. Thus, it has a false negative rate of 15-46% and a tumor undergrading rate of up to 38%.[vi]
To solve this problem, Dr. Sperling is a leader in targeted biopsy guided by real time (live) mpMRI. This is a minimal prostate biopsy yet it optimizes accuracy.[vii] With the patient lying in the bore (tunnel) of his 3T magnet, Dr. Sperling clearly identifies the area suspicious for csPCa.
He then targets a minimum number of needles (typically 2-4) into the core of the area where the most dangerous cancer cells are likely to be. Not only is it highly accurate, it greatly reduces the risks associated with TRUS biopsy, such as infection or blood in urine/semen.
The Sperling Prostate Center uses the services of a specialized pathology lab to analyze the needle samples. This means patients can be confident that the pathology report gives Dr. Sperling correct information for planning treatment with high success rates yet minimal impact of quality of life.
What are the main elements in excellent prostate cancer diagnosis?
Excellence in MRI-based diagnosis requires four main elements:
- High-quality images obtained on 3T MRI technology with integrated AI tools
- Acquiring and interpreting scans using the standardized PI-RADS reporting system
- Integrating imaging results with other key clinical factors
- If need for biopsy is indicated, real time MRI-guided targeted biopsy uses the fewest needles yet optimizes diagnostic findings.
Under Dr. Dan Sperling’s direction, the top tier Sperling Prostate Center provides all four elements. Coupled with Dr. Sperling’s decades of experience and success, his powerful 3 Tesla magnet allows for best detection of clinically significant prostate cancer while potentially identifying patients who can safely avoid immediate biopsy.
Frequently Asked Questions
Q: How do Dr. Sperling’s diagnostic services help make a treatment plan?
A: Dr. Sperling points out that thorough diagnosis is important for treatment planning because each patient’s disease, lifestyle and personal preferences are unique. Since most prostate cancer is found when it is still localized (contained in the gland), it is essential to map the location, size, chape and biology of a patient’s prostate tumor in order to match treatment to the disease. This avoids overtreating low risk cancer, or undertreating higher risk cancer.
Q: What are the basic treatment choices?
A: Generally speaking, treatment choices range from most aggressive to least aggressive. As a rule of thumb, the more aggressive the treatment, the greater the risk of post-treatment urinary, sexual or bowel side effects.
- Whole gland (radical) treatments are the most aggressive, and include surgery to remove the gland plus some surrounding structures if needed, radiation (beam or seed implants), and ablation (destruction) by extreme heat or cold. Radical treatment is usually prescribed for intermediate to high risk localized prostate cancer.
- Less than whole gland (sub-radical) treatments, such as ablating the half of the gland that contains the cancer while sparing the other side of the gland. Sub-radical treatment is not recommended for high risk localized prostate cancer.
- Focal treatment ablates (destroys) the tumor plus a safety margin surrounding the treatment zone. Focal treatment for qualified patients may be used for low- to favorable intermediate-risk disease.
- Active Surveillance is a method to delay treatment while monitoring the cancer using periodic PSA (and/or other) tests and mpMRI, as prescribed by the doctor. If monitoring signals increased cancer activity, biopsy results may trigger a move to treatment.
Content reviewed by Dr. Dan Sperling, M.D., DABR — updated November 2025
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Ziayee F, Schimmöller L, Boschheidgen M, Kasprowski L et al. Benefit of dynamic contrast-enhanced (DCE) imaging for prostate cancer detection depending on readers experience in prostate MRI. Clin Radiol. 2024 Mar;79(3):e468-e474.
[ii] Glemser PA, Netzer N, Ziener CH, Wilhelm M et al. Improving risk stratification of PI-RADS 3 + 1 lesions of the peripheral zone: expert lexicon of terms, multi-reader performance and contribution of artificial intelligence. Cancer Imaging. 2025 Aug 19;25(1):102.
[iii] Salinas-Miranda E, Birosh A, McInnes MDF, Breau RH et al. NPV of Biparametric and Multiparametric Prostate MRI: A Comparative Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 2025 May;224(5):e2432328.
[iv] Bodar YJL, Zwezerijnen BGJC, van der Voorn PJ, Jansen BHE et al. Prospective analysis of clinically significant prostate cancer detection with [18F]DCFPyL PET/MRI compared to multiparametric MRI: a comparison with the histopathology in the radical prostatectomy specimen, the ProStaPET study. Eur J Nucl Med Mol Imaging. 2022 Apr;49(5):1731-1742.
[v] Hamm CA, Asbach P, Pöhlmann A, et al. Oncological Safety of MRI-Informed Biopsy Decision-Making in Men With Suspected Prostate Cancer. JAMA Oncol. 2025;11(2):145–153.
[vi] Descotes, JL. Diagnosis of prostate cancer. Asian J Urol. 2019;6(2): 129-36.
[vii] Schimmöller L, Blondin D, Arsov C, Rabenalt R et al. MRI-Guided In-Bore Biopsy: Differences Between Prostate Cancer Detection and Localization in Primary and Secondary Biopsy Settings. AJR Am J Roentgenol. 2016 Jan;206(1):92-9.