KEY TAKEAWAYS:
How does multiparametric MRI improve prostate cancer diagnosis?
Multiparametric MRI (mpMRI) uses three imaging sequences—T2-weighted, diffusion-weighted, and dynamic contrast enhancement—to identify suspicious prostate tissue with high accuracy. By clarifying abnormal PSA results before biopsy, mpMRI can reduce unnecessary procedures and improve detection of clinically significant cancer. This noninvasive, radiation-free method is becoming the standard for early, precise diagnosis.
mpMRI helps patients by:
- Clarifying suspicious PSA results
- Reducing unnecessary biopsies
- Improving the accuracy of PCa diagnosis
- Guiding a targeted biopsy for most accurate diagnosis
Why does accurate early detection of prostate cancer matter?
Prostate cancer (PCa) treatments are a leading cause of side effects that affect a patient’s quality of life. On the other hand, if left untreated, PCa is a leading cause of cancer-specific death among men. The earlier PC is caught and treated, the greater the likelihood for successful cancer control. Most men will remain disease-free. The goal is to effectively treat the cancer with minimal side effect risks.
Achieving the goal lies in early detection and accurate diagnosis to qualify patients for less invasive treatments. At Sperling Prostate Center, multiparametric MRI (mpMRI) is used to clarify PSA screening results before biopsy.
Will the PSA screening test tell me if I have prostate cancer?
Screening for PCa is a way to find cancer that may be at risk of spreading before spread has started. This is called early detection. PSA screening (blood test) is a the most common screening method to identify men who may may have PCa. However, the PSA test is not specific because it can mean other things.
A number of noncancerous conditions can also cause a suspicious rise in PSA. It is very important to clarify a suspicious result before prescribing an invasive needle biopsy. This is because biopsy has its own risks of pain, side effects, and inaccurate diagnosis (21-47% false negative rate).
How does multiparametric MRI clarify a PSA test result?
Thankfully, noninvasive magnetic resonance imaging (MRI) can clarify a suspicious PSA test before biopsy. Similar to X-rays or CT scans that use radiation, mpMRI shows tissue inside the body but uses no radiation.
The most accurate scanning method is called multiparametric MRI (mpMRI). It is becoming a new standard of care because it may allow 27% of patients to avoid a biopsy. Parameter means a sequence or setting, and multi means 3 or more. mpMRI of the prostate uses three parameters because cancer has different characteristics from healthy tissue. Each parameter reveals a distinct cancer feature.
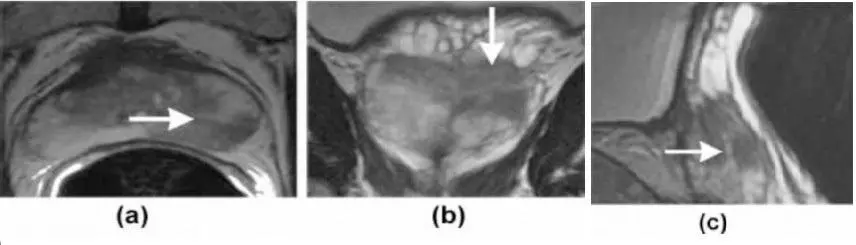
To identify PCa, three MRI parameters are combined: T2 weighted imaging, Diffusion Weighted Imaging (DWI), and Dynamic Contrast Enhancement (DCE).
What does T2 weighted imaging show?
T2 weighted imaging has been called the “work horse” of mpMRI. It shows prostate anatomy (size and shape of the gland, its three interior zones, neighboring structures, and any suspicious tissue changes within the prostate). This information is combined with the next two parameters.
What does Diffusion Weighted Imaging do?
The second parameter, Diffusion Weighted Imaging (DWI), enhances what T2 weighted shows. It detects the motion of water molecules in tissues. PCa is denser than healthy tissue, so it restricts motion which DWI reveals. Before reaching a final conclusion, a third sequence helps validate T2 weighted and DWI.
What does Dynamic Contrast Enhancement add?
Dynamic Contrast Enhancement (DCE) is the third parameter. It adds confidence that cancer is present. A contrast agent highlights areas of increased blood flow, which tumors rely on to grow.
Thus, when the same lesion is anatomically visible, restricts water motion, and has increased blood flow, it is highly likely that PCa is present.
If a biopsy is needed, what’s the most accurate method?
When a radiologist has a high degree of certainty that the mpMRI scan has detected PCa, a needle biopsy is needed to diagnose the tissue itself. A biopsy is the best diagnostic method because the actual cancer cells can be examined under a microscope. Here is another area in which mpMRI stands out.
A conventional transrectal ultrasound (TRUS) guided biopsy uses at least 12 needles to sample the gland because ultrasound cannot “see” tumor tissue. Instead, mpMRI guidance targets a minimal number of needles precisely into the core of the suspicious area where the more aggressive PCa cells are likely to be harbored. The Sperling Prostate Center specializes in real time (in-bore) MRI guided targeted biopsy.
Thus, the laboratory analysis of the cells can give the greatest diagnostic accuracy. A 2020 study confirmed that real time (in-bore) mpMRI targeted biopsy had the highest accuracy rate, noting that real-time MRI guidance is “optimal for the diagnosis of anterior and central lesions.”
Frequently asked questions (FAQ)
Q: My PSA test came back higher than usual. Should I be worried?
A: Don’t worry, because several noncancerous conditions can cause a rise in PSA. Ask your doctor about a repeat PSA test to rule out lab error and to check your PSA density (PSA-d). It it’s still suspicious, we recommend having a multiparametric MRI scan. Even if it is negative for cancer, you now have baseline for future comparisons if needed.
Q: Does it hurt to have a multiparametric MRI?
A: This type of MRI is noninvasive, safe and painless. You will have an injection into a vein in order to deliver a contrast agent for one of the imaging sequences. If you have any concern or fear about injections, talk to your doctor before the scan.
Q: If the MRI shows a tumor, why can’t I just have it treated? Why do I need a biopsy?
A: It is not responsible to treat what appears to be a tumor without more specific information. Only an analysis of the actual cells allows a treatment to be planned that best matches the cancer location, aggression level, and the extent of its involvement.
Q: If it turns out I have prostate cancer, what’s my next step?
A: Stay calm. When prostate cancer is diagnosed early, it is highly treatable, and 5-year success rates are nearly 100%. You and your doctor will discuss your biopsy results, your MRI scans, and other clinical factors such as your age, family history, lifestyle, etc. and any other test results your doctor ordered. The goal is to control the cancer with minimal-to-no impact on your lifestyle. The more thorough your diagnosis, and the more experienced your doctor, the greater likelihood it can be achieved.
Content reviewed by Dr. Dan Sperling, M.D., DABR — updated October 2025.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.


