You lie calmly on your back in the tunnel (bore) of a large machine. You can’t feel it, but you are now in an invisible magnetic field. After a while, your scanning session is done. Abracadabra! Presto! Such is the magic of Magnetic Resonance Imaging (MRI) that your doctor can examine and analyze your gland in amazing detail, with no exposure to radiation as in x-rays or CT scans. The next thing you know, your doctor is showing you his findings and discussing what they mean. Amazing!
“In the realm of modern medical diagnostics, few technologies have revolutionized the way we perceive the human body as profoundly as Magnetic Resonance Imaging (MRI). Since its inception, MRI has emerged as an indispensable tool in healthcare, enabling clinicians to delve deep into the body’s intricate structures without invasive procedures or ionizing radiation,” writes pathologist Dr. W Wang.[i]
So, if it’s not magic, exactly how does it work?First of all, the magnetic field itself does not produce the images, but it sets up a base by aligning your body’s protons (subatomic particles) with its field. This creates a state of equilibrium. The field can be modulated by applying gradients, and the equilibrium of the protons is altered by pulsing a type of electric signal called radiofrequency into the field. This process can produce loud noises, so patients wear special ear protection during MRI—but the actions of the field and radiofrequency pulses are absolutely harmless for the patient.
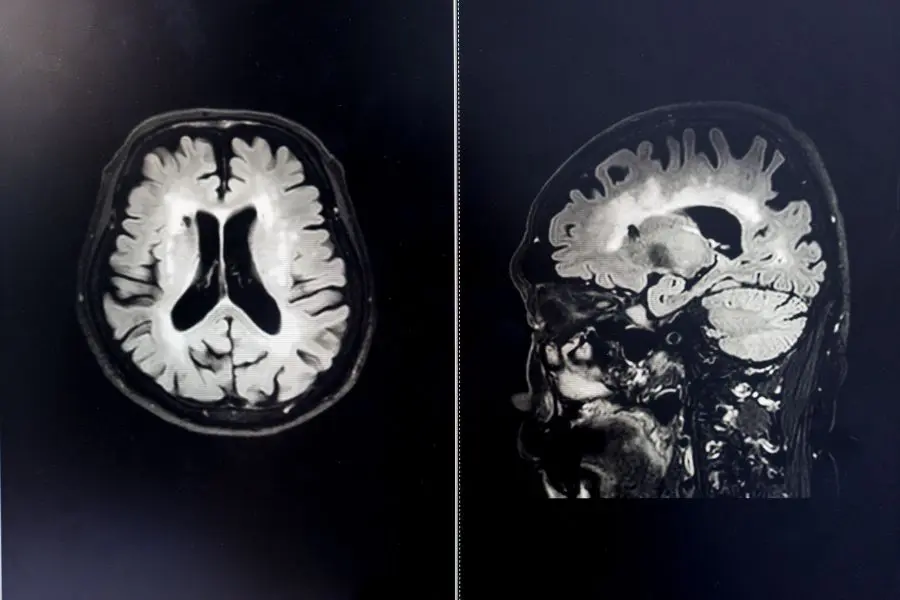
As the proton alignment responds to alterations in the field, it generates a “signal” that is sent to special software that converts signal intensity to black-and-white images. Intensity varies depending on the substance, e.g. fluid, fat, type of tissue, etc. as well as the gradient-radiofrequency combination. On a screen, this will show up as areas ranging from bright white to black, and everything in between. For example, here is a brain/head scan revealing diagnostic details:
For today’s MRI of the prostate, we capture multiple types of visual information by using three different imaging sequences, or parameters—thus the term multiparametric MRI, or simply mpMRI. Each sequence differs from the others based on gradient modulations, and the pulse sequence and direction.
Here are the three sequences we use, and the type of visual information each provides:
- T2-weighted (T2W) – This reveals the anatomy and structure of the gland in three dimensions. The gland is made up of zones that can be identified on T2W, and areas of suspicious looking structures will be different in appearance from healthy tissue. Suspicious areas are called regions of interest.
- Diffusion-weighted imaging (DWI) – This is another way to identify regions of interest based on the movement of water molecules in tissue. Denser tissue such as a prostate cancer tumor restricts water motion, and this can be “quantified” on DWI sequences.
- Dynamic contrast enhancement (DCE) – This is the third way to detect tumor activity based on its unique blood flow. Tumors build their own blood vessels to provide them with the oxygen and nutrients they need for their cells to thrive and multiply. These are not orderly like normal blood vessels, but are chaotic. The patient is given an IV injection of a contrast agent that flows with the blood to the prostate. As it moves in and out of any tumor blood vessels, it will show up and be tracked during this imaging sequence, revealing suspicious tumors and other unusual inflammation in the gland.
When an experienced reader interprets all sequences, the region of interest is clear. It is given a PI-RADS score ranging from 1 (highly unlikely to be cancer) to 5 (highly likely to be cancer). Any PI-RADS score of 2 or more warrants a biopsy, preferably a real-time MRI-guided biopsy targeting 2-4 needles directly into the region of interest. Research shows this is the least invasive yet most accurate biopsy.
Thus, mpMRI of the prostate is not magical. It is, however, practically miraculous in its powers of early detection. Identifying suspicious areas as soon as possible offers patients the greatest chance of treatment success. Not only that, but early detection means higher odds that the patient will qualify for a focal treatment—another example of medical engineering’s power to amaze!
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Wang W (2023) Unveiling the Wonders of Magnetic Resonance Imaging (MRI). J Imaging Interv Radiol. 6:07. https://www.primescholars.com/articles/unveiling-the-wonders-of-magnetic-resonance-imaging-mri-122679.html