KEY TAKEAWAYS:
MRI-guided Focal Laser Ablation treats localized prostate cancer by destroying only the tumor while preserving urinary and sexual function. As practiced by Dr. Dan Sperling, Focal Laser Ablation offers cancer control comparable to radical treatments while providing better preservation of urinary, sexual and bowel function. This approach balances cancer control with quality of life.
At the Sperling Prostate Center, precision image-guided Focal Laser Ablation optimizes survival and quality of life, thanks to:
- Real-time MRI planning
- Accurate targeting of laser beam energy
- Thermometry software to monitor and confirm treatment.
Does Focal Laser Ablation balance cancer control with quality of life?
Progress in treating prostate cancer is shaped by goal of optimizing survival while minimizing side effect risks. If treatment side effects compromise urinary, sexual or bowel function, a patient’s quality of life may suffer and the patient may regret his decision.[i]
At the Sperling Prostate Center, Dr. Dan Sperling offers precise image-guided Focal Laser Ablation. Focal Laser Ablation is designed to control cancer while minimizing damage to urinary, sexual and bowel structures. Thus, it is a prostate cancer therapy that balances cancer control with quality of life.
Is focal therapy an effective alternative to radical surgery or radiation?
Focal therapy is an effective alternative to radical (whole gland) treatments like prostatectomy or radiation. Focal therapy “provides adequate functional outcomes with oncologic control like established whole-gland therapies.”[ii]
There are several focal therapy methods. One particular method, Focal Laser Ablation, uses precision laser energy to ablate (destroy) a prostate cancer tumor while sparing key urinary and sexual structures. As practiced by Dr. Dan Sperling, it is an alternative to radical treatment for qualified patients.
What makes Focal Laser Ablation so precise?
Focal Laser Ablation is a highly precise method for ablating a prostate cancer tumor. Three important factors contribute to its precision:
- Real-time MRI guidance allows accurate treatment planning.
- Laser beam delivery is focused on the target tumor.
- Special temperature mapping software monitors and confirms the exact ablation zone.
What is the role of MRI image guidance?
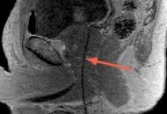
A special type of Magnetic Resonance Imaging (MRI) called multiparametric MRI (mpMRI) is used to plan, guide delivery, and confirm the effect of Focal Laser Ablation. Multiparametric MRI clearly characterizes a cancerous tumor within the prostate gland. It reveals the location, shape and extent of the tumor.
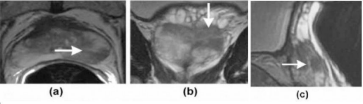
Once the target tumor is defined, the doctor can plan where to place the laser fiber in order to destroy the targeted area plus an extra safety margin. This planning includes the location and depth so the tip of the fiber is strategically placed to maximize the laser’s effect. Since the fiber is visible on MRI, the doctor knows that its placement is accurate.
How does the laser destroy cancer?
Living tissue, whether healthy or diseased, can be destroyed by extreme temperatures of heat or cold. In the case of Focal Laser Ablation, laser light is used to generate heat when the light energy is absorbed by cells. When activated, the tip of the fiber creates intensely focused, controlled heat at a high enough temperature to kill a tumor.
How is Focal Laser Ablation monitored?
The doctor can monitor the ablation as it occurs. When the laser is activated, the heat quickly expands with precise boundaries. Special MRI software called thermometry makes a temperature map of the prostate and the ablation. It shows the size and temperature of the laser-generated heat as it destroys the tumor and the safety margin. Thus, the doctor can avoid damage to nearby urinary and sexual structures, sparing normal prostate function.

When the ablation is complete, a final MRI scan is done to confirm that the targeted ablation matched the planned area. Also, multiparametric MRI can characterize the destroyed tissue, assuring there is no surviving cancer activity in the targeted area.
At the Sperling Prostate Center, our precision MRI-guided Focal Laser Ablation is a balanced solution. It helps patients achieve cancer control while preserving quality of life.
Frequently asked questions (FAQ)
Is Focal Laser Ablation an outpatient procedure?
At the Sperling Prostate Center, Focal Laser Ablation is performed as an outpatient procedure. Generally, patients have local anesthesia to numb the area and may be given oral medication for relaxation. Following the procedure, patients get dressed. There is a brief recovery time during which Dr. Sperling reviews the results of the treatment with the patient, and goes over what to expect at home.
How quickly can a patient return to normal activity?
Generally, patients resume normal work and domestic activity within a few days, though individual patient experience and preference will vary. Patients are encouraged to avoid vigorous physical activity/lifting for 1-2 weeks. Dr. Sperling makes recommendations to each patient, based on their procedure.
What are typical statistics for Focal Laser Ablation cancer control?
Although Focal Laser Ablation has been in development for over 10 years, with Dr. Sperling recognized as a leading pioneer. Medium term studies report promising results:
- 83% of patients remained free from failure (average follow-up 71 months).[iii]
- 17% needed additional treatment after one year.[iv]
What are urinary side effect rates for Focal Laser Ablation?
After any focal treatment, including Focal Laser Ablation, urinary incontinence is very rare, and if it occurs, it usually resolves within weeks.[v]
What are rates of erectile dysfunction?
Rates vary, and important to take into account the patient’s sexual function before treatment. For example, one study reported no significant difference in Sexual Health Inventory for Men (SHIM) scores before and after Focal Laser Ablation over time, with erectile dysfunction reported as grade 1 (mild) in 5% of patients and grade 2 (mild to moderate) in 2.5%. Compare this with rates after prostatectomy, which average from 50-60% at one year after surgery.
If I’m diagnosed with prostate cancer, am I a candidate for Focal Laser Ablation?
Not every patient with prostate cancer qualifies for a focal therapy such as Focal Laser Ablation. Here are the most important criteria:
- Patients should have clinically localized disease (still contained in the prostate)
- Patients should have low to favorable-intermediate risk prostate cancer (Grade Group 2, Grade Group 3 depending on other factors)
- The target tumor should be of a size that it can be encompassed by the type of destructive energy used, along with a safety margin of surrounding normal prostate tissue
- To determine if an individual’s prostate cancer is amenable to focal therapy, the Sperling Prostate Center provides multiparametric MRI on a powerful 3T magnet, as well as real time in-bore MRI-guided targeted biopsy if needed clinically significant prostate cancer is suspected.
Content reviewed by Dr. Dan Sperling, M.D., DABR — updated January 2026.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Nguyen T, Lightfoot C, May D et al. Patient Reported Outcomes and Treatment-Associated Complications as a Consideration in Selecting Localized Prostate Cancer Management. Res Rep Urol. 2025 Jun 12;17:195-210.
[ii] Sandberg M, Thole D, Nowatzke J, Underwood G et al. Focal Therapy for Localized Prostate Cancer: A Case Series with Cost Analysis. Curr Oncol. 2025 Aug 23;32(9):476.
[iii] Chao B, Lepor H. 5-Year Outcomes Following Focal Laser Ablation of Prostate Cancer. Urology. 2021 Sep;155:124-129.
[iv] Walser E, Nance A, Ynalvez L, Yong S et al. Focal Laser Ablation of Prostate Cancer: Results in 120 Patients with Low- to Intermediate-Risk Disease. J Vasc Interv Radiol. 2019 Mar;30(3):401-409.e2.
[v] Rakauskas A, Marra G, Heidegger I, Kasivisvanathan V et al. Focal Therapy for Prostate Cancer: Complications and Their Treatment. Front Surg. 2021 Jul 12;8:696242.


