Let’s start with a short quiz: What is the current preferred strategy to manage low-risk prostate cancer?
a) Nerve-sparing robotic prostatectomy
b) Focal treatment
c) Active Surveillance
d) Vitamin E, saw palmetto supplements, and avoid red meat
If you answered “c) Active Surveillance,” you are correct. According to a 2017 joint guideline statement from four national professional organizations (American Society of Clinical Oncology , American Urological Association, American Society for Therapeutic Radiation and Oncology, and Society for Urologic Oncology), Active Surveillance (AS) is recommended in order to avoid being treated upfront.
In recent years, the use of AS has increased from about 7% to 40%, which is encouraging since it means fewer newly diagnosed, low-risk patients are not being rushed into aggressive, whole-gland treatments. But AS is more than just watching and waiting. It requires 1) being carefully and properly qualified to make sure there is not occult (hidden) aggressive prostate cancer, and 2) committing to a prescribed protocol to monitor for tumor growth (enlargement) or progression (becoming more dangerous).
Qualifications for AS
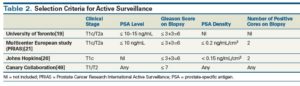
Qualifying patients for AS begins with knowing the tumor stage, PSA, and Gleason score. Depending on the source of the criteria, additional factors may include PSA density and the number of positive biopsy cores. The table below shows four different methods of qualifying patients:[i]
However, we now know that these guidelines are only about 80% accurate. This is partly because conventional TRUS biopsy method can’t visually see a tumor in order to aim at it. Thus, it can completely miss significant (potentially dangerous) prostate cancer. PSA level is also not reliable. There are aggressive prostate cancer cell lines that don’t even raise PSA – so no one suspects their presence.
More accurate qualification
There are two fairly recent developments that, when incorporated into the above clinical factors, greatly improve accurate qualification:
- Multiparametric MRI (mpMRI) performed on a powerful 3T magnet – not only does this type of scan identify and characterize prostate cancer tumors, it can also be used in real time to guide a minimum number of biopsy needles into the core of any suspicious area, providing the most accurate diagnosis, including a high probability of capturing hidden aggressive cells. In short, 3T mpMRI offers a 3-D, high resolution visual portrait of prostate cancer tumors.
- Biomarkers are microscopic clues that give detailed genomic or molecular information about a patient’s prostate cancer. According to Loeb & Tosoian (2018), “Several markers are now available that can be used to refine risk classification and help with the initial decision to pursue AS.”[ii] Depending on the testing method used, biomarkers can be obtained from blood, urine, or the tissue samples captured during the biopsy. They can identify telltale genetic mutations that signal a dangerous cancer cell line requiring prompt treatment.
When all qualifiers (scan results, biomarkers, tumor stage, PSA/PSA variants, and Gleason score) are favorable, we have a high degree of confidence that a patient is a great candidate for AS.
Monitoring promoted AS success
Once we know the patient is a great AS candidate, the next step is planning the most successful monitoring. The purpose of diligent tracking is to catch any change as soon as possible in order to avoid missing a treatment window, which constitutes a failure of AS. Many monitoring protocols still include a routine TRUS biopsy, often at the end of the first 12 months since AS began, and repeated every 1-3 years. However, “…AS strategies that rely on frequent serial prostate biopsy are associated with added patient burden and risk of side effects. Of particular concern is the increase in infectious complications after biopsy, corresponding with a rising prevalence of antimicrobial resistance in the community.”[iii]
The Sperling Prostate Center joins other international experts in the belief that 3T mpMRI plus PSA blood tests is the foundation of successful monitoring. Repeat biopsy should only be done if the combination of imaging and blood test detects a suspicious change. If so, an MRI-guided targeted biopsy reduces the risks and unpleasantness associated with repeat biopsies.
We believe in AS for the right patient. We believe in identifying the right candidate carefully. And we believe in monitoring using the right tools. If you want Active Surveillance success, do it the right way.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] [i] Garisto J, Klotz L. “Active Surveillance for Prostate Cancer: How to Do it Right.” Cancer Network, Vol. 31, Issue 5. http://www.cancernetwork.com/oncology-journal/active-surveillance-prostate-cancer-how-do-it-right
[ii] Loeb S, Tosoian J. Biomarkers in active surveillance. Transl Androl Urol. 2018 Feb; 7(1): 155–159.
[iii] Ibid.