What is the Safest MRI Contrast Agent?

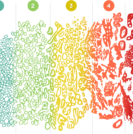
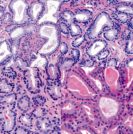
Contrast agent Before addressing the title question regarding safety, it’s important to understand what a contrast agent does during MRI prostate imaging. Multiparametric MRI (mpMRI) of the prostate relies on two or more imaging sequences, or parameters, each of which depicts certain tissue characteristics that the others do not. When the results are synchronized, we keep reading