MRI-Guided Biopsies
The Sperling Prostate Center offers a targeted MRI-Guided biopsy of suspected prostate tumors using two types of procedures:
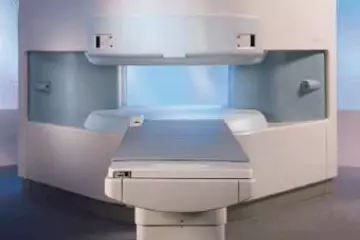
- MRI-Guided Biopsy – Using advanced MRI images of a suspected tumor/tissue, Dr. Sperling performs a targeted prostate biopsy inside the MRI gantry.
- MRI/TRUS Fusion Biopsy – First an advanced MRI prostate image is obtained, annotated and recorded by the Sperling Prostate Center. Next, using special fusion technology, the recorded MRI image is fused with a live transrectal ultrasound by the Urologist who performs a MRI/TRUS fusion biopsy.
Why MRI-Guided Prostate Biopsy
For the last two decades, transrectal ultrasound (TRUS) guided biopsy has been used to diagnose prostate malignancy based on what’s been referred to as a “blind” procedure.
It’s blind because specific prostate tumors, especially very small ones, cannot always be distinguished by ultrasound due to its poor resolution of soft tissue. In addition, TRUS biopsies based on a systematic approach tend to target the peripheral aspects of the gland and are likely to miss 30-40% of prostate cancer located in the anterior, midline transition zone, or apex1. Today, however, many tumors are being identified at a very early stage, often as extremely small lesions that are hard to spot on ultrasound and hard to sample using a TRUS biopsy alone.
Commonly, these small, early stage tumors are at a level of risk that might not necessarily threaten a patient’s life. On the other hand, some prostate cancer cell lines are very dangerous. Thus, the question arises about which treatment is the best for each individual case.
What patients want is clear, reliable information that will help them and their doctors make an accurate diagnosis. Likewise, if prostate treatment is determined to be the best course of action, the choice of that treatment will depend on many factors, especially the nature of the prostate cancer identified during a patient’s biopsy.
Today’s next generation, advanced MRI technology combined with the proprietary protocol of the Sperling Prostate Center uses high-resolution 3D images that can distinguish between normal and diseased tissue to help precisely pinpoint potential cancerous cells within the prostate. The result is better ability to identify and characterize prostate malignancy1, especially important in today’s changing landscape of smaller, lower risk tumors.
An MRI-Guided Biopsy is highly targeted to select tissue revealed by the MRI imaging. That means physicians and patients have the confidence that any tissue samples come from locations identified as having the most likely chance of containing cancer. The result is a targeted approach vs. the “blind” approach of a TRUS biopsy.
In addition, our Radiologists at the Sperling Prostate Center typically need only 2 or 3 biopsy samples rather than the 12-14 needles commonly used for a standard transrectal ultrasound (TRUS) biopsy (or the possible 60 needles used for some transperineal saturation biopsies).
MRI Prostate Biopsy Highlights
- With advanced MRI imaging techniques, a prostate biopsy can be performed within the MRI gantry to target suspected tumor(s).
- Our Radiologist typically takes 2 or 3 samples rather than the 12-14 needles used for a TRUS biopsy or the even greater number of needles used for a saturation biopsy.
- The procedure is targeted and patients find it generally more comfortable than a traditional TRUS biopsy.
- This procedure can be performed in place of a TRUS biopsy or following a TRUS Biopsy when more accuracy is desired.
Sperling Prostate Biopsy Protocol
- Imaging: Multi parametric MRI prostate scans to provide precise details about the size and dimensions of the prostate gland. In addition, several sophisticated tests (including T2-weighted and diffusion-weighted contrast) are performed during the MRI to help identify the location and size of potential cancerous tumors. Additionally, an endorectal coil image with contrast enhancement is used to further distinguish between normal and diseased tissue.
- Computer Enhancement: Computer-aided software helps to identify abnormal areas as shown through the enhancement activity. Any suspicious tissue found is annotated for an MRI-Guided Biopsy.
- Targeting: The MRI-Guided biopsy is used to target a specific area(s) for biopsy. A tiny needle guide is used to precisely locate potential cancerous cells within the prostate.
- Sampling: Once the MRI image is obtained and the abnormal tissue is identified, a needle is inserted through the guide to the targeted area for tissue sampling.
- Precision: The device used to perform the MRI-Guided biopsy establishes its own frame of reference from the patient’s initial set of images. The images are used to locate suspicious areas in the prostate gland and then are correlated with the new images obtained at the time of biopsy for targeting. This type of biopsy requires less sampling because of its precision targeting.
- Pathology: Biopsy samples are sent to a pathology lab for analysis. As with traditional biopsies, the test results are typically available a few days after the MRI biopsy is performed. The Sperling Prostate Center uses state-of-art pathology to grade and stage any cancerous tissue/tumors sampled. This includes the use of molecular markers such as PCA3 and new gene sequence tests to help better understand the aggressiveness of the cancer. The pathology findings provide the final confirmation of prostate cancer and help us identify both the volume of cancer and the level of risk (or aggressiveness) the cancer presents.
- Prostate Mapping: The patient’s MRI scans are combined with pathology findings to confirm the location, size and aggressiveness of any confirmed tumors. The end result is a detailed prostate MAP that provides the best possible tumor information along with a blueprint for treatment selection and treatment planning. The prostate MAP also identifies the precise location of sensitive structures that the physician can leave untreated if no cancer is discovered (e.g. the neurovascular bundles).
- Treatment Planning: The primary value of Prostate MAP is to provide valuable information for treatment planning and follow up. Our goal is to provide patients and physicians with extensive and detailed information that can help determined the best course of action, including the best choice of treatment, and execute that treatment.
Who Should Consider a Prostate MRI-Guided Biopsy
- Patients with a rising PSA level yet negative biopsy. The detailed informationprovided by MRI can lead the doctor to the area most suspicious for disease, thereby increasing the chance of obtaining a comprehensive biopsy.
- Patients who have experienced a biopsy one or more times and want to improve the sensitivity of diagnosis for cancer, if present
- Patients looking to identify the precise size, location and extent of prostate cancer
- Patients looking to help confirm the stage and grade of their prostate cancer
- Patients looking to determine if their cancer is confined to the prostate, or if it has spread outside the walls of the prostate gland
- Patients who choose to monitor a low level of prostate cancer in order to hold off on treatment
- A patient’s radiation treatment therapy can be planned, as it is important that the radiation be concentrated on the affected area. An MRI can provide a clear picture in helping the oncologist guide the therapy that is most appropriate for a particular patient.
- Patients who are considering a radical prostatectomy, including a robotic procedure. An MRI can provide a clear picture in helping the urologists to guide the surgery to be effective while reducing morbidity.
- Patients considering an ablation, including Laser, Cryoablation or HIFU
- Patients considering a focal or targeted ablation treatment
- Patients who have a local recurrence, indicated by a high PSA level, following a radical prostatectomy, radiation, Cryoablation, HIFU or Laser Ablation. MRI can evaluate the entire area for abnormal tissue.
MRI-Guided Prostate Biopsy Risks
Biopsy Risks
A prostate biopsy has a slight risk of causing problems such as:
- Infection. This is more common in men who have undiagnosed prostatitis. Usually, taking antibiotic medication before the biopsy prevents an infection from developing.
- Bleeding into the urethra or bladder. This can cause a blood blister (hematoma), an inability to urinate, or a need to urinate often.
- Bleeding from the rectum. If you have a transrectal biopsy, you may experience a small amount of bleeding from your rectum for 2 to 3 days after the biopsy.
- An allergic reaction to the anesthetic medications used during the biopsy.
Note: A prostate gland biopsy does not typically cause any long term problems with erections and will not make a man infertile.
MRI Risks
- The MRI examination poses almost no risk to the average patient when appropriate safety guidelines are followed.
- Although the strong magnetic field is not harmful in itself, implanted medical devices that contain metal may malfunction or cause problems during an MRI exam.
- There is a very slight risk of an allergic reaction if contrast material is injected. Such reactions usually are mild and easily controlled by medication. If you experience allergic symptoms, a radiologist or other physician will be available for immediate assistance.
- Nephrogenic systemic fibrosis is currently a recognized, but rare, complication of MRI believed to be caused by the injection of high doses of gadolinium contrast material in patients with very poor kidney function.
- Ahmed HU, Kirkham A et al. Is it time to consider a role for MRI before prostate biopsy?. Nat Rev Clin Onc . 6. 197-206. (2009).