“Look before you leap.” That advice originated centuries before you first heard it at a kid. Its first known use was found in a 1350 Latin manuscript. Then in 1546 it appeared in English from a collect of proverbs. It was good wisdom back then. Today, it’s even better wisdom if a PSA blood test is abnormally high. That’s because PSA might be a red flag for prostate cancer (PCa), but it might now. How can you know?
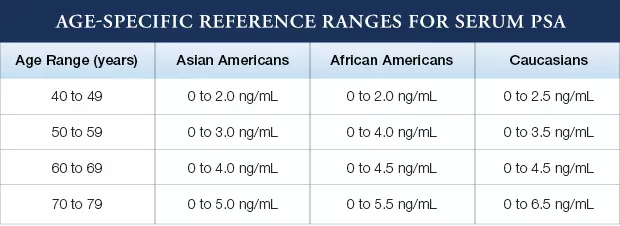
Take a look at “normal” PSA numbers, which differ based on age and ethnicity. As our website shows:
The problem is not the blood test itself, but how most urologists have been trained to respond to a rising or high PSA. They generally recommend having an immediate conventional biopsy of 12-14 needles guided by transrectal ultrasound (TRUS). This type of biopsy is like firing a shotgun into a dark room, so it tends to over-detect insignificant PCa (does not require immediate or aggressive treatment) and under-detect significant PCa (can become life-threatening if left untreated or under-treated). Plus, there are side effect risks from so many needles (pain, infection, blood in urine or semen, even ED).
Some urologists may buy more time before biopsy by advising the patient to have a repeat blood draw in a few weeks or months. They want to rule out the possibility of a temporary stimulus such as having sex or riding a bike the day before, as well as the possibility of lab error.
In the event, however, that the second PSA remains elevated, the patient is now urged to have a biopsy ASAP. Should he make the leap? The answer lies in first taking a look before making a decision.
MRI before biopsy reveals the unknown
An original study now provides compelling evidence that multiparametric MRI before biopsy offers a highly accurate view of the patient’s prostate, which will inform the biopsy decision. The paper, “Combined MRI and PSA Strategy Improves Biopsy Decisions Compared with PSA Only…”, was published in September, 2022.[i] The research was based on 881 patients suspected of PCa based on a PSA test and prebiopsy MRI. For this analysis, no patient had a PSA greater than 20, and all patients were either biopsied or clinically followed for 2 years to diagnose the presence of PCa.
Here are the numbers: 220 men were diagnosed with clinically insignificant PCa, while 162 were found to have clinically significant PCa. These findings were retrospectively correlated with PSA only, and then with combined PSA + mpMRI.
The authors found that PSA alone had relatively low predictive value. Why? It’s because “PSA increases not only in prostate cancer, but also in the presence of benign prostatic hyperplasia or prostatitis,” as well as after certain activities that can stimulate the gland. Instead, they found that adding MRI to PSA can “greatly improve” the detection of clinically significant disease, which warrants a biopsy. They report that this protocol was consistently superior to PSA alone for determining biopsy necessity, for both gray area PSA results as well as high PSA.
The authors conclude by noting that “…this longitudinal observational study confirmed that adding prebiopsy MRI to PSA was consistently beneficial in patients with PSA ≤ 20 ng/mL for avoiding unnecessary biopsy…”
Thus, prebiopsy mpMRI is the essential “look before you leap” before making a biopsy decision. Fortunately, a growing number of urologists are beginning to embrace a diagnostic pathway that includes a referral for MRI imaging before prescribing a biopsy. Unfortunately, if a biopsy is mandated based on detection of clinically significant disease, many still don’t recognize the value of referring the patient to an expert prostate radiologist for a real time, in-bore MRI-guided targeted biopsy, such as we offer at the Sperling Prostate Center. The clear advantage of this approach is its precision diagnosis using a minimum number of needles vs. a TRUS biopsy.
If you or someone you know has recently received a suspicious PSA blood test result, contact us for information on how our excellent services can help.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
References
[i] Choi MH, Ha US, Park YH, Hong SH et al. Combined MRI and PSA Strategy Improves Biopsy Decisions Compared
with PSA Only: Longitudinal Observations of a Cohort of Patients with a PSA Level Less Than 20 ng/mL. Acad Radiol. 2022 Sep 17:S1076-6332(22)00417-2.


