Understanding the PI-RADS Score and What it Means for You
PI-RADS Score Simply Explained – To Biopsy or Not To Biopsy?
PI-RADS is a rating scale for the likelihood that clinically significant prostate cancer (PCa) is present. It is a 5-number system, from least likely to most likely:
| Very low risk. Clinically significant cancer is highly unlikely to be present. | |
| Low risk. Clinically significant cancer is unlikely to be present. | |
| Intermediate risk. Clinically significant cancer may or may not be present. | |
| High risk. Clinically significant cancer is likely to be present. | |
| Very high risk. Clinically significant cancer is highly likely to be present. |
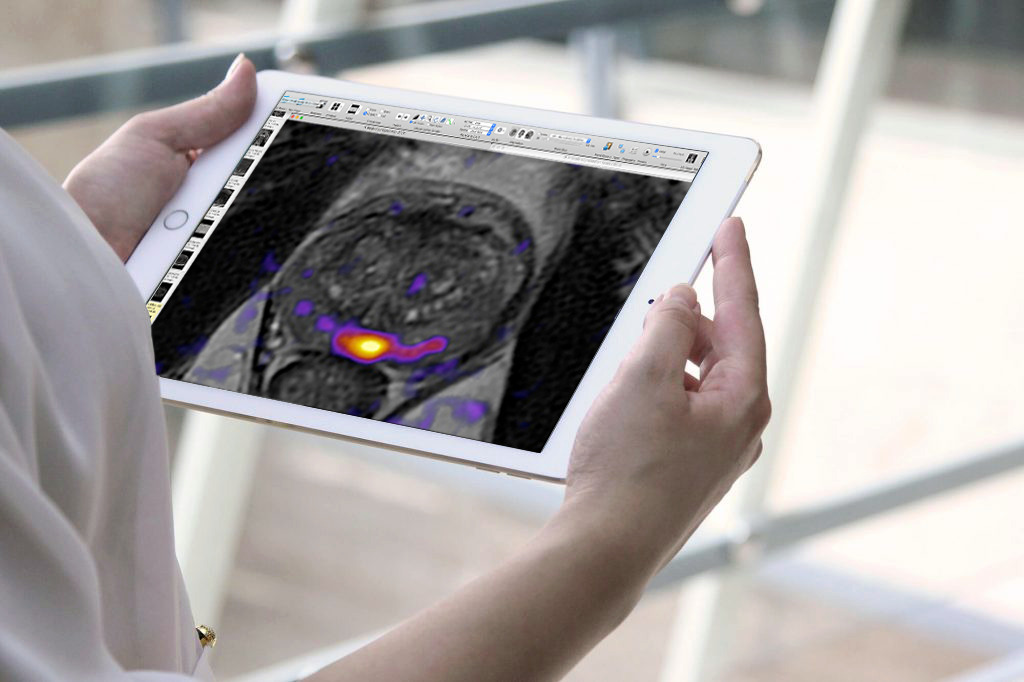
The PI-RADS system was developed by a panel of prostate imaging specialists. Its purpose was simple: improve agreement among radiologists who interpret prostate MRI scans by providing detailed, standardized descriptions of what imaging sequences to use, and how PCa shows up in each sequence. Since 2011 when the first version was published, there have been two more versions. Each version, based in biology and technology advances, has increased reader accuracy, especially among experienced radiologists like Dr. Sperling who specialize in prostate imaging.
Suspicion of Prostate Cancer?
A free consultation with Dr. Sperling will help find out if a biopsy is necessary. If it is, our MRI-guided system is the safest, most accurate method available.
Is PI-RADS the same as Gleason score and Grade Group?
There are three current scales used to “rank” the danger of PCa. They are parallel but not identical, since each gives important information in slightly different ways. Compare the slight differences:
| Designed by radiologists to help radiologic readers identify significant PCa on mpMRI. See above explanation for each PI-RADS score, which reports the likelihood that significant PCa is present. | Designed by a pathologist who recognized 5 different patterns (grades) of PCa cells as seen under a microscope. Gleason score is always shown as the sum of 2 numbers (e.g., 3+4=7) based on the 2 highest proportions of the most aggressive pattern in each biopsy needle sample. The 2-number sum can be confusing for patients. | “1 is the new 6” – a simplified version of the Gleason grade system designed by urologists to help patients understand risk level GG1 – low risk (Gleason score 3+3=6) GG2-favorable intermediate risk (Gleason score 3+4=7) GG3- unfavorable intermediate risk (Gleason score 4+3=7) GG4 – high risk (Gleason score 4+4=8) GG5 – high risk (Gleason score 9 or 10) |
The benefits of PI-RADS
To understand the important benefits of PI-RADS for you, keep in mind that before mpMRI, the only pathway to diagnose PCa was invasive because it went straight from a suspicious PSA blood test result to a 12+ needle biopsy guided by transrectal ultrasound (TRUS). Not only does TRUS biopsy have risks (infection, bleeding, pain, etc.) but it has at least a 30% error margin. It over-detects insignificant cancer, and often misses significant cancer, leading to treatment mismatch, side effects and poor outcomes.
In today’s new pathway, men with suspicious PSA results can take advantage of an intermediate step before biopsy: mpMRI. When performed by an expert on a powerful magnet, the PI-RADS score can make the difference between biopsy not needed (PI-RADS 1 or 2) or biopsy needed (PI-RADS 3, 4 or 5). Studies show that, with mpMRI and PI-RADS, up to 50% of patients will not need a biopsy at the time of the scan.[i]
What if PI-RADS means a biopsy is necessary?
If PI-RADS shows likelihood of clinically significant cancer, a needle biopsy is the only responsible way to make a diagnosis because it’s based on actual tissue examined under a microscope. If PCa is present, knowing its exact location, shape, size and aggression is the secret to best treatment outcomes.
The Sperling Prostate Center provides the best biopsy method available. Once the PI-RADS score shows a biopsy is needed, our real time, in-bore MRI targeted biopsy excels in all areas:
- Since the suspicious area is seen in real time, MRI guidance allows precise targeting.
- Targeting uses a minimal number of needles to sample the area(s) likely to harbor the most dangerous cells, which facilitates planning the most appropriate treatment.
- Real time MRI is more accurate than fusion-guided biopsies because it’s done in real time while the patient lies in the opening of the magnet (this is what in-bore means). Fusion biopsies are subject to error so their targeting falls short of real time MRI targeting. To make up for this, fusion biopsy is most often accompanied by additional systematic needle sampling.
Experience matters

It’s equally important to get an expert interpretation of what can appear to be PI-RADS 4 or 5, but may not in fact be cancer. While most of the time it means aggressive PCa is present, a small number of men will turn out to have a benign but possibly precancerous condition such as PIN or ASAP. Dr. Sperling is able to identify this, thanks to our state-of-the-art magnet, assistance from Artificial Intelligence tools, and his own diagnostic skill.
Dr. Sperling’s ability to read MRI scans knowledgeably is not only beneficial for our Center’s patients, but when Dr. Sperling reviews outside scan results sent to him for a second opinion, it’s not unusual for him to discover missed PI-RADS lesions, or even upgrade the previous report. While this may be disappointing for the patient, it means his treatment choice can be adapted to suit the danger level of his PCa—which avoids shocking news months or years later if cancer comes back. Every man with suspected PCa can benefit from mpMRI interpreted by Dr. Sperling.
For more information, or to schedule a prostate mpMRI exam or review of previous results, contact our Center.
Take the Next Step Today
Request your free consultation with Dr. Sperling and we’ll work together to create the best diagnostic plan for you.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
style=”text-align:center;”
[i] Venderink W, van Luijtelaar A, van der Leest M, Barentsz JO et al. Multiparametric magnetic resonance imaging and follow-up to avoid prostate biopsy in 4259 men. BJU Int. 2019 Nov;124(5):775-784. doi: 10.1111/bju.14853. Epub 2019 Jul 23. https://www.ncbi.nlm.nih.gov/pubmed/31237388