Focal Laser Ablation for Benign Prostatic Hyperplasia (BPH)
What is Benign Prostatic Hyperplasia?
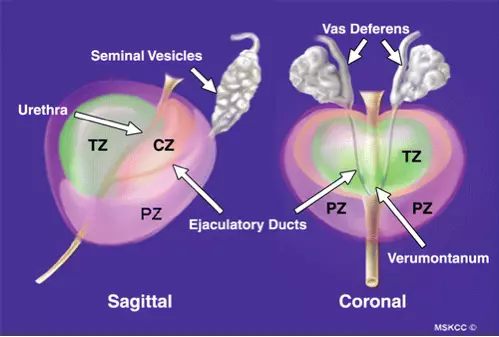
Benign Prostatic Hyperplasia is a normal non-cancerous enlargement of the prostate gland that occurs as men age. The types of tissue that make up the three prostate zones gradually change. The risk of BPH increases as a man grows older. Roughly 20% of men in their fifties experience BPH; 60% of men in their sixties have it, and by age ninety it affects 90% of men.
BPH Problems
Many patients are able to reduce symptoms through changes in behavior (e.g. reduced fluids before bedtime, dietary changes to exclude bladder irritants). Also, many supplements carry claims of easing symptoms, but research shows contradictory results; most studies conclude there is no significant benefit. As symptoms increase, patients may turn to prescription medications that can reduce symptoms. While this is now the most common BPH treatment, long term side effects are still being studied.
If drugs are not effective, surgical procedures to widen the urethra will be recommended. Such procedures are called transurethral, meaning instruments are inserted through the penis into the urethra (tube that carries urine out of the bladder) where it passes through the prostate gland, in order to physically widen the urethra. Examples are TURP, TUMT, TUNA, and transurethral laser delivery systems. See Frequently Asked Questions at the end for more details.
Because most of these interventions basically damage the lining of the urethra, healing can take up to several weeks. Side effect risks vary with each procedure.
The Sperling Solution
Dr. Dan Sperling, a leading expert in target ablation of prostate tumors, is the world’s leading pioneer in applying Focal Laser Ablation to treat Benign Prostatic Hyperplasia.
The Sperling Prostate Center offers a unique new FDA-cleared approach to treating BPH. With the same kind of MRI-guided Focal Laser Ablation (FLA) used to treat prostate cancer tumors, Dr. Dan Sperling has developed a patient-friendly outpatient treatment that relieves BPH in a single treatment with minimal side effects. After FLA, as the ablated tissue shrinks, pressure on the urethra passage is reduced naturally.
Identifying and targeting BPH
Before treatment, BlueLaser™ 3T mpMRI is used to produce a very high resolution, 3-D prostate scan of the three prostate zones to identify the TZ tissue areas to be ablated, and plan the best approach to the target.
A special case: enlarged median lobe of the prostate
In most BPH cases the tissue enlargement is somewhat uniform throughout the gland. However, there is another type of BPH that affects only a small, cone-shaped section of the gland called the median lobe, near the bladder neck. When BPH causes selective overgrowth of the median lobe, it can indent or squeeze the bladder neck, creating a mechanical blockage to urine flow.
An important point about median lobe BPH is that it is unlikely to respond to medication. Nor may such patients be candidates for conventional transurethral procedures. Focal laser ablation is an intervention that “unblocks” the interfering tissue by focusing on it precisely, giving maximum effect with minimal discomfort, short healing time, and few short term side effects.
Treating BPH with Focal Laser Ablation
Once the gland has been mapped out and the treatment path is planned, Focal Laser Ablation for BPH (FLA-BPH) relieves BPH-related urinary symptoms by reducing the enlarged TZ (transition zone) tissue causing urinary blockage. This process is called debulking because it diminishes the bulky BPH tissue. The ablation is done with the type of laser that coagulates, not vaporizes, tissue. By ablating targeted areas of the transitional zone near but not touching the urethra, FLA-BPH creates strategic tissue shrinkage by generating harmless scar tissue that will be reabsorbed by the body. There are minimal-to-no residual urinary or sexual side effects because the treated areas are contained well within the prostate gland away from other healthy tissues and structures. (Based on the location and extent of FLA, some patients may wear a catheter for several days to protect the urethra as inflammation diminishes.) The urinary symptoms of BPH begin to diminish within a few weeks as the resulting scar tissue is reabsorbed by the body.
FLA-BPH side effects
There are little-to-no long term side effects from FLA-BPH (as there can be with intraurethral ablation procedures) because in most cases we are not damaging the urethral lining. Erectile function is spared because the TZ is within the prostate and not adjacent to the nerves that control erection. Finally, the side effect called retrograde ejaculation (semen flowing backward into the bladder) that can occur after TURP or Green Light laser is much less likely after FLA-BPH. NOTE: As with transurethral procedures, minimal transient (short term) side effects may occur after FLA-BPH, but these tend to resolve quickly.
Advantages of FLA-BPH
- Outpatient procedure
- No general or spinal anesthesia, only local numbing
- Real-time guidance using our BlueLaser™ 3T mpMRI
- Nothing inserted into the penis or urethra
- The only focal treatment for median lobe BPH at the bladder neck
- One-time treatment with excellent results
- Little-to-no residual side effects
- Can accommodate larger gland sizes effectively
Frequently Asked Questions
How is BPH diagnosed?
In addition to a complete medical history, there is a special questionnaire called the International Prostate Symptom Score (I-PSS) that screens for BPH and other possible prostate conditions. To rule out other prostate diseases, the doctor might conduct any or all of the following tests:
- Urinalysis
- Blood test, including PSA, free PSA or PSA density
- Urinary flow test
- Post-void residual volume test (any urine left in the bladder after urination)
- Urodynamic studies (water introduced into the bladder through a catheter to measure internal pressure and bladder contractions)
- Cystoscopy (insertion of a thin scope for visual inspection of the urethra and bladder)
- Imaging using a contrast dye to reveal aspects of the urinary system
We highly recommend having a 3T multiparametric MRI of the prostate (when interpreted by an experienced radiologist, it will clearly show BPH and/or median lobe obstruction).
How is Focal Laser Ablation for BPH (FLA-BPH) different from transurethral procedures?
FLA-BPH is performed under real-time BlueLaser™ 3T mpMRI guidance instead of a visual scope or ultrasound guidance. Unlike transurethral procedures that access the urethra through the penis, a small laser fiber optic is inserted precisely into the center of each area to be treated under real-time MRI guidance. During each 2-3 minutes of laser activation, special software shows temperature changes in the tissue being treated, assuring there is no heat damage to surrounding tissues. Following ablation, the MRI is used to confirm each ablated area. After the procedure is done, the patient meets with Dr. Sperling during a brief recovery, and then leaves. The entire procedure is thus completely different from transurethral procedures such as TURP, TUMT, TUNA, other transurethral laser procedures, Resum therapy, and Urolift®.
Some of the other procedures also use laser. Are there different lasers?
Our Focal Laser Therapy is called laser interstitial thermal therapy. It is different from the types of laser used to widen the urethra. Those are delivered through the penis into the urethra, and have a vaporization effect on tissue. On the other hand, laser fiber optics, inserted directly into organ or gland tissue, have a very precise coagulation effect that results in scar tissue. Total gland volume is reduced as the scar tissue is gradually and harmlessly reabsorbed by the body.
What is Transurethral Resection of the Prostate (TURP)?
TURP is a surgical procedure done under anesthesia in which the surgeon uses a very small instrument inserted into the urethra through the penis in order to scrape away excess prostate tissue. It usually involves 1-3 days in the hospital. Some patients call it “reaming out.” Healing may take up to 3 weeks or more. Side effects: difficulty controlling urine stream, erectile dysfunction, retrograde ejaculation (semen flows backward into the bladder), urinary blockage, and infertility.
What is Transurethral Microwave Thermotherapy (TUMT)?
TUMT is a 1 hour outpatient procedure that uses an antenna inserted into the urethra through the penis to generate sufficient heat to destroy overgrown tissues without damage to healthy tissues. Depending on prostate anatomy, not everyone is a candidate. May take time to produce results.
What is Transurethral Needle Ablation (TUNA)?
TUNA uses a needle to deliver radiofrequency energy to destroy tissue. It is usually done as an outpatient procedure under local, general or spinal anesthesia. A catheter is worn while the urethra heals. Possible side effects: blood in urine, painful urination, difficulty urinating, risk of infection.
What is indigo laser therapy?
To perform indigo laser therapy, a very slender probe with a laser delivery system at the tip is introduced through the urethra. It can be done outpatient under local or regional anesthesia. The type and strength of laser energy used causes coagulation (clumping and scarring) of small volumes of dead tissue, which are eventually passed off through the urethra. While there are very few side effects, patients wear a catheter for several days to a week so the passage of dead tissue does not block urine flow. Improvement in symptoms may occur over 6-12 weeks.
What is laser vaporization therapy (Green Light Laser or KTP laser)?
A cystoscope is used to introduce a laser fiber that generates another type of laser energy. This type vaporizes, rather than coagulates, prostate tissue. It is done outpatient under anesthesia. Side effects may be similar to TURP, though with less severity; healing is shorter than with TURP.
What is Rezum therapy?
Rezum therapy (convective radiofrequency water vapor thermal therapy) is a type of TUNA that uses very hot water vapor (steam) to destroy cells along the urethral lining. The body gradually absorbs the dead tissue, alleviating BPH symptoms. It is not yet widely available and there are no studies to show that it will continue to provide relief beyond two years. Side effects are similar to those of TUNA.
What is Urolift®?
This is a surgical implant system. A series of tiny permanent implants along the length of the prostatic urethra hold the enlarged tissue back so it does not compress the urethra, allowing better urine flow out of the bladder. It is fairly new, and long-term effects are not yet known. In about 10% of patients removal of implants that protrude into the bladder is required as they can lead to stone formation. Another 30% of patients either resume or start medications for enlarged prostate after treatment with Urolift.
End your BPH Struggle
We welcome the opportunity to answer your questions and help you craft a personalized path to wellness. Contact us today to schedule a free consultation and say goodbye to your BPH struggle.