MRI Ultrasound Fusion Guided Biopsy
Ultrasound and MRI are the two main types of imaging used to aid prostate cancer diagnosis, and the use of multiparametric 3T MRI presents a major advancement in prostate cancer detection and diagnosis because of its superior imaging ability over ultrasound alone. Fusion is a process that blends these technologies to create a detailed, 360° prostate map by merging previously captured MRI images with live TRUS images while the ultrasound wand is inserted. Only a very small number of U.S. urologists have the necessary knowledge, equipment and software to practice fusion imaging. Dr. Dan Sperling is one of those specialists.
The correct descriptive term for this type of imaging is “MRI Ultrasound Fusion Guided Biopsy.” However, other terms are frequently used and refer to the same process. These terms include Fusion-Guided Biopsy, Fusion Biopsy, MRI/US Biopsy, MRI-Ultrasound Fusion Biopsy, and simply MR Fusion Biopsy. Because these terms can be confusing, we prefer the technically correct name for this procedure.
For a more detailed version of this page, please visit MRI-guided Biopsy vs. Fusion: What’s the Difference?
How does it work?
A urologist must be specially trained to read prostate MRI and identify the area of interest (suspected tumor). The urologist must also “segment” or input the prostate outline into the computer to facilitate matching MRI and TRUS shapes. Special software is necessary that can recognize both types of images, assign “coordinates” to each type, and match (register) the images, coordinate by coordinate. This is called image registration or co-registration, and it overlays the live TRUS image onto the static MRI image. The result a synthetic 3D image of the patient’s gland that is quite accurate, but not perfect, due to small variables such as patient movement or inaccurate segmentation. The final 3D image can be manipulated on the computer screen so the urologist can view it from every angle, and the suspicious area is highlighted within the image.
To get the idea, imagine you insert several photos of your face from various angles into a computer that can scan and read them. Now imagine a friend taking a video all around your face, and the video image inputted into the same computer, which matches the live video with the still photos. The computer now blends all the images and creates a 3D view of you that looks like a Pixar image of yourself. Your friend can use the computer mouse to rotate the Pixar image of you from different angles. The resemblance may be quite remarkable, but there may be some slight differences or distortions.
Prostate MRI Ultrasound Fusion imaging is done in the urologist’s office to help identify the target area for the biopsy and guide needles into it.
Is It Accurate?
Experts agree that targeted MRI Ultrasound Fusion Guided Biopsies are generally more accurate than traditional TRUS biopsies (ultrasound only) in detecting and diagnosing prostate cancer. Depending on the software or fusion device, the computer may help plan the sampling based on the target area(s) within the gland as depicted in the fused images. The urologist using fusion technology can follow the plan or override it. This includes the number of needles and angle of approach. The real-time TRUS verifies the placement of the needles, which show up on the monitor.
Comparison of MRI-guided biopsy vs. fusion-guided biopsy
| MRI-guided biopsy | MRI Ultrasound Fusion Guided Biopsy |
|
|
Conventional detection methods
Prostate ultrasound
Prostate ultrasound is done using a wand inserted into the rectum. Thus, it is called Transrectal Ultrasound, or TRUS. The wand transmits soundwaves through the rectal wall toward the prostate gland. The waves bounce off of different kinds of tissue, and register as black-and-white images on a computer monitor. Although abnormal prostate tissue may show up differently than normal tissue, the information about the true nature of the abnormality is limited.
TRUS-guided biopsy
Traditionally, prostate needle biopsies have been performed by urologists under ultrasound guidance.
| Upside | Downside |
|
|
Our advantage
Prostate multiparametric 3T MRI
Experts agree that MRI is the most sensitive imaging technique of all currently available imaging technologies. Today’s features include a number of parameters that reveal much more than just prostate anatomy, revealing clearer visual definition of even small prostate cancer tumors or other abnormalities. For example:
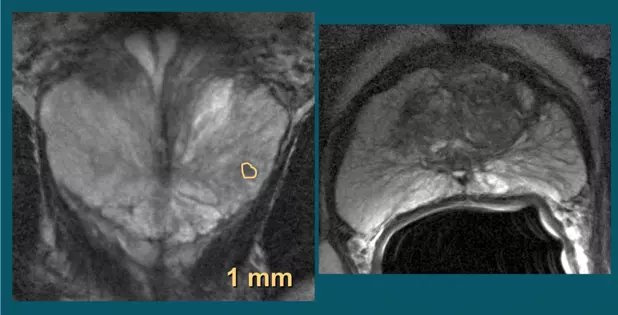
- Diseased (pathologic) tissue shows up as anatomical differences (T2 weighted imaging)
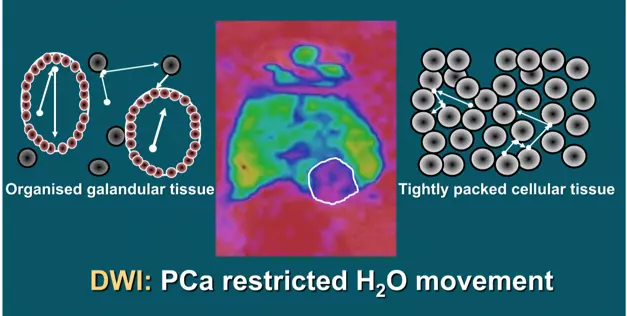
- The movement of water molecules in tumor cells differentiates them from normal cells (diffusion weighted imaging or DWI)
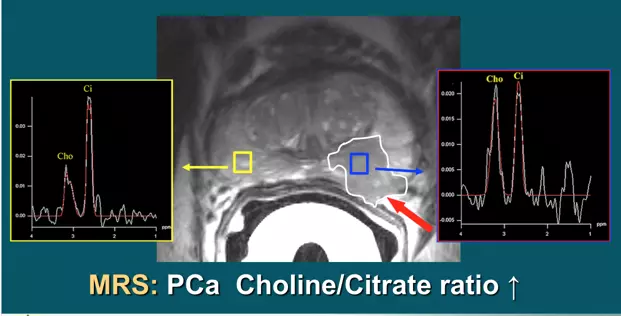
- The presence of certain chemicals (metabolites) in tumor cells distinguishes them from healthy cells (spectroscopy or MRI-S)
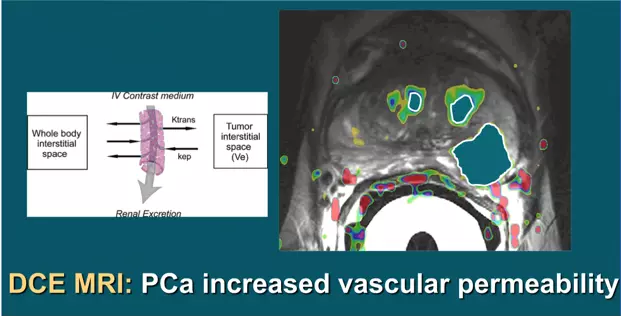
- Changes in the uptake and washout of contrast agents characterizes cancer cells (dynamic contrast-enhanced imaging or DCE)
In addition to these multiparametric indicators of a cancer, our powerful 3T (3 Tesla) magnet provides very high resolution of tumors.
According to an authoritative Dutch center, “Multiparametric (mp)-MRI has been shown to be highly accurate in detecting and localizing intermediately aggressive and highly aggressive cancers.” However, they emphasize that the experience of the radiologist conducting prostate MRI is critical in capturing the images and correctly interpreting them.
Studies designed to correlate tumors identified by (mp)-MRI in pre-prostatectomy patients confirm the accuracy of the MRI images when read by an experience radiologist, as compared to surgically removed prostate specimens.
Fig. 2a: T2 weighted images show suspected tumor activity
DWI images detect water molecule motion in cancerous tissue even at microscopic levels
Spectroscopy improves the definition of cancer by revealing the presence of certain chemicals that indicate malignancy
DCE shows changes in the uptake and washout of an injected contrast agent by cancer cells
The Sperling Prostate Center offers two key advantages for excellence in detection and diagnosis:
- State-of-the-art 3T MRI with the most advanced multiparametric software
- Dr. Dan Sperling‘s top-tier experience in prostate MRI and MRI-guided biopsies
MRI-guided biopsy at Sperling Prostate Center
A biopsy done under real time MRI guidance in the bore (tunnel) of the magnet, especially by an expert, is the most precise and efficient biopsy available.
| Upside | Downside |
|
|
Summary
The Sperling Prostate Center offers patients the safest, most efficient and accurate biopsy process available. Guided by real time 3T multiparametric images, under the direction of the radiologist with most U.S. experience in MRI-guided biopsies, the results offer a significant degree of confidence over other biopsy methods. As van de Ven and Barentsz point out, “Direct MRI-guided biopsy is likely to the most accurate technique as it is less prone to fusion and motion errors.” It is our belief that the MRI Ultrasound Fusion Guided Biopsy is a positive addition to the field of urology, helping urologists bring targeted biopsies into their practice. However, we also believe that MRI imaging done live, in real time, has no substitute. There is no need for a “middle man” like the fusion process, with the extra steps (and therefore room for some distortion). Live MRI imaging, read and interpreted by recognized prostate MRI expert Dr. Dan Sperling, is quickly becoming the preferred prostate biopsy guidance that can best inform decisions for tailored prostate cancer treatment.